Abdominal aortic aneurysms (AAA) are life-threatening serious conditions that require effective and quick management. Although it is generally acknowledged that patients with AAA obtain the greatest benefit from endovascular repair (EVAR) compared to open surgical repair (OSR), there are few comparisons between the surgical approaches in Western versus Chinese patients. We aimed to perform a meta-analysis of studies in which EVAR was compared with OSR in the management of abdominal aortic aneurysms. We searched the Western literature through PubMed, OVID and Web of Science from 1991 until December 2018 and the Chinese-language literature from 1998 until December 2018. We pooled the results in January 2019 based on standardized inclusion and exclusion criteria and analyzed them using a conventional meta-analysis. Forty-five English papers with 31,074 AAA patients and twenty-one Chinese studies with 1,405 patients were included in this study. Chinese subjects were more likely to undergo endovascular repair than Western subjects (44.5% versus 41.5%, P = 0.012). The 30-day post-discharge mortality rate in Western studies was significantly lower for EVAR than for OSR (odds ratio (OR) = 0.481, P < 0.001). However, there was no significant reduction in the 30-day mortality rate following EVAR compared to OSR (OR = 0.733, P = 0.425) for Chinese patients. In Western patients, the postoperative complication rate of respiratory system and cardiac system was lower in the EVAR group than in the OSR group (OR = 0.270, P < 0.001 and OR = 0.411, P < 0.001, respectively), nevertheless, for Chinese patients, limb ischaemia was more common (OR = 1.539, P = 0.049) in the EVAR group. Whether in Western patients with an eight-year follow-up period or Chinese patients with a maximum four-year follow-up period, there was no significant difference between the EVAR and OSR groups in the all-cause death rate (hazard ratio (HR) = 1.026, P = 0.483 and HR = 1.173, P = 0.247, respectively). Chinese patients were more likely to receive EVAR than OSR and the 30-day mortality was significantly lower for EVAR than for OSR in Western patients but not in Chinese patients. Endovascular repair can be applied to Chinese patients with a reasonable safety margin. Further work is needed to explore the causes of these treatment differences.
The abdominal aortic aneurysm (AAA) is one of the most common silent killers in elderly men. Rupture of an abdominal aortic aneurysm is usually fatal. Endovascular repair (EVAR) techniques and especially elective repair have been applied in the treatment of abdominal aortic aneurysms both in Western countries (i.e., Europe and North America) and China (Adriaensen et al., 2002; Lovegrove et al., 2008). Most randomized controlled trials comparing EVAR and open surgical repair (OSR) were conducted in Europe (De Bruin et al., 2010) and North America. In contrast, scant data are available in Chinese populations. As OSR use expands to new regions as an alternative method to EVAR, questions regarding its usage in non-Caucasian patients have been raised.
A meta-analysis by (Adriaensen et al., 2002) examined short-term discrepancies between EVAR and OSR using data which were described as non-randomized prospective or retrospective data. A subsequent meta-analysis (Lovegrove et al., 2008) ameliorated this data limitation, but its long-term (more than five years for EVAR) results were not convincing. The EVAR cure rates are controversial with regard to medium-and long-term outcomes, such as all-cause mortality, aneurysm-related mortality and re-intervention. The recent Dutch Randomized Endovascular Aneurysm Management (DREAM) (De Bruin et al., 2010) and EVAR-1 trial results (United Kingdom EVAR Trial Investigators et al., 2010) with regard to EVAR versus OSR have shed light on long-term outcomes. Specifically, six years after randomization, EVAR and OSR of abdominal aortic aneurysm resulted in similar survival rates. The rate of secondary interventions was significantly higher for EVAR than for OSR.
More importantly, the prevalence of AAAs is different in Western and Chinese populations. Additionally, the promotion of EVAR occurred later in China than in Western countries. Although the results of domestic studies (Fu et al., 2003) confirmed that EVAR is suitable for Chinese patients, three areas based on domestic studies are still inconclusive: 1) the Chinese morbidity rate, 2) the morphological specificity of aneurysms and 3) a diameter of aneurysm ≥ 5.5 cm as indication for the domestic treatment of abdominal aortic aneurysms. Although it is generally acknowledged that EVAR accords greater benefit than OSR to AAA patients, studies comparing the two techniques in Western versus Chinese populations are sparse. Furthermore, short term outcomes in EVAR versus OSR were not confirmed by meta-analyses based on Chinese patients. Consequently, material for the comparison of both treatments is still lacking.
To better understand the effects of EVAR in Chinese populations, we analyzed data on AAA repair from the literature published during the period that EVAR was introduced. Thus, the aim of our current investigation was to carry out a systematic review of the studies in which EVAR was compared to OSR in the treatment of AAAs patients from Western countries (North America and Europe) and China.
A systematic literature search of Western articles on EVAR and OSR of infrarenal AAA was carried out by two independent researchers (Y. H and J. Z) using the MEDLINE (PubMed), journals@Ovid Full Text, and BIOSIS previews databases (OVID). The following Medical Subject Headings (MeSH) search terms were used: aortic aneurysm, abdominal, vascular surgical procedures, stents, and randomized controlled trial. In addition, exploding keywords included endovascular, comparative, and mortality. The corresponding search strategy is provided (Supplementary files 1). We limited our search to reports on human subjects in the English language. We searched databases for articles published between November 1991 (because (Parodi et al., 1991) published their results on the first clinical application of endovascular repair for abdominal aortic aneurysm in 1991) and December 2018. Every relevant article retrieved had its references thoroughly checked. Following this the articles were entered into the ISI WEB OF KNOWLEDGE: WEB OF SCIENCE database (1991 to 2018) to find the references cited in order to find any related literature. Relevant medical journals were also thoroughly checked.
We performed a comprehensive search of the Chinese literature. The key words abdominal aortic aneurysm and endovascular repair were used in a comprehensive search of the CBMdisc (Chinese Biomedical Database) and CNKI (Chinese National Knowledge Infrastructure) databases. All Chinese studies on abdominal aortic aneurysm treatment between January 1998 (because in 1998, Jing and colleagues (Jing et al., 1998) published their initial article of endovascular repair AAA in China) and 24th December 2018 were identified. Reference lists were also examined and relevant articles added to the list. Furthermore, several Chinese journals were hand searched from 1998 to 2015, specifically the Chinese Journal of Practical Surgery, Chinese Journal of General Surgery, Chinese Medical Journal, and Chinese Journal of Vascular Surgery.
Inclusion criteria: Randomized controlled, prospective, and retrospective, studies were included if they met the following criteria:
(a): patients diagnosed with an infrarenal and non-ruptured abdominal aortic aneurysm undergoing elective endovascular repair were compared with patients undergoing elective open surgical repair;
(b): at least 20 patients;
(c): sufficient data (> 25 percent of predefined variables) such as patient baseline characteristics and short- and long-term outcomes;
(d): in the case of multiple reports from the same institution, only the most rigorous published report was used to avoid duplication of data;
(e): however, when two or more studies from the same institution reported on medium- or long-term outcomes on the same patients, the results from all linked studies were included synergistically.
Excluded criteria: articles were excluded if they:
(a): did not report outcomes in a comparable fashion;
(b): included patients with other aortic pathologies such as ruptured abdominal aortic aneurysms, thoracic aortic aneurysms and aortic dissections;
(c): contained insufficient data (< 25 percent of predefined variables);
(d): did not meet the criteria for abstracts and unpublished data;
(e): were confined to select subgroups of patients (e.g. octogenarians).
Complications were classified and graded according to the reporting standards of the Ad Hoc Committee for Standardized Reporting Practices in Vascular Surgery of the Society for Vascular Surgery International Society for Cardiovascular Surgery. Three classes of complications (systemic, local-nonvascular, and local-vascular or implant-related) and three grades of severity (mild, moderate, and severe) were used. A reintervention was defined as any surgical or endovascular procedure that was related to the primary aneurysm-repair procedure.
We aimed to reduce the possibility of publication bias through the following methods: searches of meeting abstracts, theses, dissertations and contacting authors for any additional unreported data. When necessary, we contacted the authors of the original papers to receive further information. The risk of bias was assessed using the methods of (Lundh and Gøtzsche, 2008).
Randomized controlled trials (RCTs): the quality of the methodology was assessed independently by two reviewers (F.S. and Y.H.) using the Cochrane risk of bias tool (Higgins et al., 2011). The risk of bias was divided into low (all criteria met), moderate (one or more criteria met), and high (no criteria met). In addition, the quality of the methodology used in each study was evaluated by the same authors, using the system described by (Jadad et al., 1996). Non-randomized studies (NORS): The quality of non-randomized studies was assessed by two reviewers (F. S. and Y. H.) using the MINORS scoring system describe by (Slim et al., 2003). This method uses (Moher et al., 1999) items for comparative studies with each item scored 0, 1 or 2 corresponding to not reported, inadequately reported, and adequately reported, respectively. Whether RCTs or NORS, discrepancies in ratings were resolved by discussion between the two reviewers (C. J. and Y. H.). Additionally, when discrepancies arose, a third party (J. Z.) was consulted.
After the initial assessment for eligibility, two authors (H. Y. and S. W.) independently abstracted the data from the primary sources. They independently reviewed all the articles. Different results between the two authors were resolved by consensus. For each study we extracted rudimentary information including author(s), study design, journals published, geographical location, date published, etc. The following predefined variables were recorded using an electronic extraction form: preoperative characteristics and postoperative outcomes (we conducted a separate meta-analysis for two different postoperative time periods: short-term and mid-long term). Follow-up visits were scheduled 30 days and 12, 24, 36 months and 5 years after the procedure. Any death or complications occurring within 30 days after the original procedure were defined as short-term, and any death, complication and reintervention occurring more than 30 days after the original procedure were defined as mid-long term. For the results during the follow-up period in the long-term analysis we used data on all-cause mortality at 1, 2-3 and more than 5 years after discharge, the rate of re-intervention at 1 year and more than 4 years and aneurysm-related mortality at 2-3 years and more than 5 years.
This study was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (available at http://www.prisma-statement.org/) This study was also conducted in accordance with the Quality Reporting of Meta-analyses (QUROM) guidelines (Moher et al., 1999) and reporting Meta-analyses of observational studies (MOOSE) guidelines (Stroup et al., 2000). We measured the odds ratio (OR) for dichotomous data, reported with 95% confidence intervals (CI). In addition, we calculated the weighted mean difference (WMD) with 95% CI for continuous data. The analysis was performed by comparing EVAR with OSR; an OR greater than 1 denoted that an event was more common following EVAR. We used the fixed effect model if evidence of nonsignificant heterogeneity was found. If there was evidence of significant heterogeneity, a random effects model as described by (DerSimonian and Laird, 1986) was used, and the degree of heterogeneity was assessed using the I2 (Lovegrove et al., 2008) test. I2 (Lovegrove et al., 2008) values of 25%, 25-50% and >50% were considered to represent small, medium and large amounts of inconsistency.
A comparison between Western and Chinese cohorts using the method of subgroups was performed to analyze the diversity between the two groups. However, for the mid-long term survival outcomes the hazard ratios (HRs), Kaplan-Meier survival curves and log-rank test P value (Tierney et al., 2007) were extracted from individual studies. Furthermore, pooling of individual log HRs was performed using the method described by (Parmar et al., 1998) Subgroup analysis and HRs which were calculated by a statistical method were used to contrast the two cohorts. An HR less than 1 indicated a better survival rate for EVAR.
Publication bias was assessed using a funnel plot. Furthermore, to assess heterogeneity, Egger’s test (Egger et al., 1997) and graphical exploration with Egger’s regression asymmetry plot were used to evaluate publication bias. We used the results of 30-day mortality and all-cause mortality for mid-long term as the effect index, because this was the most standardized outcome presented in most studies.
A difference for P < 0.05 was considered statistically significant. All statistical analyses were conducted using spreadsheet software (Microsoft Excel 2007; Microsoft, Redmond, Washington, USA) and performed using the meta. ado module of STATA (version 11.0, College Station, Texas, USA)
The Western literature search identified 172 studies for potential inclusion in the meta-analysis; 127 of these papers were excluded: 96 did not compare endovascular repair (EVAR) with open surgical repair (OSR), four papers described only a selected patient subgroup such as obese or octogenarian patients, another 18 papers contained insufficient data, and nine overlapped with included studies from the same institution. Thus, 45 papers met our inclusion criteria. Trial flow charts are provided in Fig 1. The trial flow chart for Chinese language articles is provided in Fig 2.
 Figure 1.
Figure 1.Flow diagram of this meta-analysis in accordance with the QUOROM statement from Western studies.
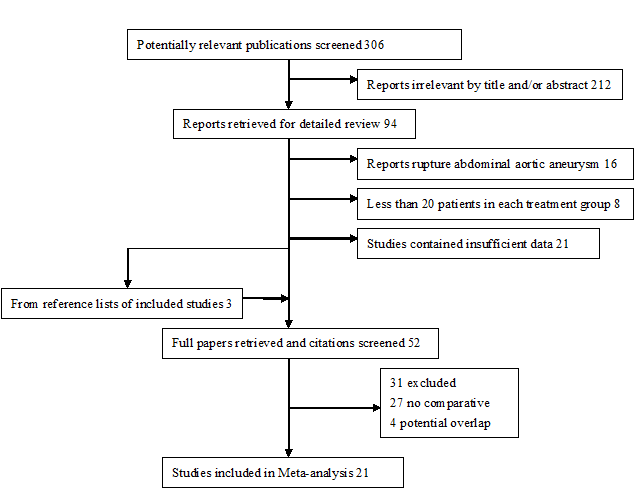 Figure 2.
Figure 2.Flow diagram of this meta-analysis in accordance with the QUOROM statement from Chinese studies.
Details of the selected articles for this study are given in Table 1 for the English language articles. The included 45 papers assessed outcomes following elective AAA repair: three reports from the Dutch Randomized Endovascular Aneurysm Management (DREAM) Trial study (De Bruin et al., 2010; Blankensteijn et al., 2005; Prinssen et al., 2004) and 3 articles from the EVAR trial 1 study (United Kingdom EVAR Trial Investigators et al., 2010; EVAR trial participants, 2005; Greenhalgh et al., 2004) were treated as one study each for the purpose of analysis because in each case one of the reports represented a mid-long term follow-up study subsequent to an initial report. In addition, because (Johnson et al., 2006) and (Bush et al., 2006), Carpenter (Carpenter and Endologix, 2004) and (Wang et al., 2008; Matsumura et al., 2003; Peterson et al., 2007) reported from the same institution; they were treated as one for the purpose of analysis. The former dates were replenished respectively by Bush, Wang and Peterson, consequently these both fitted into our study. In total, 38 studies published up to January 2011 ultimately met our predefined inclusion criteria. These articles were published from June 1998 to June 2010 and used patients enrolled from 1994 to 2007. These articles consisted of four randomized controlled trials, 12 prospective non-randomized trials, and 22 retrospective conducted studies; 13 were from Europe and 25 were from North America.
| Study | Year of Publication | Study Period | Study Location | Journal of Publication | No. of Institutions | EVAR | OSR | Study Design | Follow-up EVAR | Follow-up OSR | Comments |
|---|---|---|---|---|---|---|---|---|---|---|---|
| McNally et al | June, 2010 | 2004. 7-2007. 7 | USA | J.Vasc. Surg. | single-center | 173 | 228 | Retro. | … | … | |
| Jetty et al | March, 2010 | 2002. 4. 31-2007. 3. 31 | Canada | J.Vasc. Surg. | multicenter | 888 | 5573 | Retro. | 5 | 5 | CIHI-DAD Database $ |
| Turnbull et al | March, 2010 | 2002. 2. 25-2003. 4. 14 | USA | J.Vasc. Surg. | 13 centers | 166 | 243 | PNR | 5 | 5 | eLPS £ |
| Steinmetz et al | January 8, 2010 | 1999. 1-2006. 12 | France | Eur. J. Vasc. Endovasc. Surg. | single-center | 148 | 134 | Retro. | 5 | 5 | Include High-risk exclude low-risk |
| Chisci et al | 2009 | 2005. 1-2007. 12 | Italy and Sweden | J.Endovasc. Ther. | 2 centers | 74 | 61 | Retro. | 1.6 | 2.1 | Exclude Fenestrated EVAR |
| Dick et al | March. 29. 2008 | 1998. 1-2002. 12 | Switzerland | World. J. Surg. | single-center | 68 | 244 | Retro. | 4. 6 | 4. 9 | Exclude emergency OSR |
| Cronenwett et al | December, 2007 | 2003. 1-2006. 12 | USA | J.Vasc. Surg. | 9 hospitals | 495 | 667 | PNR | 1 | 1 | VSGNNE Database† |
| Faizer et al | June, 2007 | 1999. 1-2004. 12 | USA | J.Vasc. Surg. | single-center | 304 | 558 | Retro. | … | … | |
| Chan et al | March, 2007 | 1997. 1-2005. 10 | UK | Int. J. Clin. Pract. | single-center | 157 | 329 | Retro. | … | … | |
| Aljabri et al | December, 2006 | NG | Canada | J. Vasc. Surg. | single-center | 43 | 33 | PNR | 0.5 | 0.5 | |
| Sicard et al | August, 2006 | NG | USA | J. Vasc. Surg. | 5 IDE‡ | 565 | 61 | Retro. | 2.7 | 2.5 | High-risk |
| Johnson et al | March 15, 2006 | 2001. 5. 1- 2003. 9. 30 | USA | Am.J.Surg. | 123 VA hospitals | 717 | 1187 | Retro. | 1 | 1 | VA-NSQIP Database‖ |
| Bush et al | January, 2006 | J.Am.Coll.Surg. | |||||||||
| Aarts et al | August 2, 2005 | 1998.10-2004. 1 | Netherlands | Ann. Vasc. Surg. | single-center | 99 | 116 | Retro. | 1.9 | 1.9 | |
| Vogel et al | August 1, 2005 | 1998-2003 | USA | Ann. Vasc. Surg. | single-center | 92 | 126 | PNR | … | … | Short Form 36 (SF-36) |
| Soulez et al | August, 2005 | 1998. 9-2002. 7 | Canada | J. Vasc. Interv. Radiol | single-center | 20 | 20 | RCT | 2.4 | 2.3 | |
| Lifeline Registry | July, 2005 | NG | USA | J. Vasc. Surg. | 4 IDE‡ | 2063 | 334 | Retro. | >5 | >1 | AnCure, AneuRx, Excluder , PowerLink |
| Hua et al | March, 2005 | 2000.1. 1-2003. 10. 31 | USA | Am. J. Surg. | 14 centers | 460 | 582 | Retro. | … | … | NSQIP-PS Database¶ |
| Goueffic et al | 2005 | 1995. 1-2001. 12 | France | J. Endovasc. Ther. | single-center | 209 | 289 | PNR | 1.6 | 3.3 | |
| Carpenter et al | November, 2004 | 2000. 7. 18-2003. 3. 31 | USA | J. Vasc. Surg. | 15 centers | 192 | 66 | PNR | 1 | 1 | PowerLink |
| Wang et al | September, 2008 | 4.1 | 3.1 | ||||||||
| Cao et al | November, 2004 | 1997. 1-2003. 12 | Italy | J. Vasc. Surg. | single-center | 534 | 585 | PNR | 2.8 | 2.9 | |
| DREAM (Prinssen) | October, 2004 | 2000. 11-2003. 12 | Netherlands | N. Engl. J. Med | 24+4 centers§ | 171 | 174 | RCT | … | … | Dutch Randomized Endovascular Aneurysm Management (DREAM) Trial Group |
| DREAM (Blankensteijn) | June 9, 2005 | 2 | 2 | ||||||||
| DREAM (Bruin) | May 20, 2010 | 6 | 6 | ||||||||
| Garcia-Madrid et al | October, 2004 | 1997. 3-2000. 8 | Spain | Eur. J. Vasc. Endovasc. Surg. | single-center | 53 | 30 | Retro. | 1.6 | 2.2 | |
| Rigberg et al | September, 2004 | 2001. 1-2002. 12 | USA | Arch. Surg. | single-center | 61 | 89 | Retro. | … | … | |
| EVAR trial 1 | August 25, 2004 | 1999. 9. 1-2003. 12 | UK | Lancet. | 34 centers | 543 | 539 | RCT | … | … | The EVAR trial participants |
| June 25, 2005 | 2.9 | 2.9 | |||||||||
| May 20, 2010 | 1999. 9. 1-2004 | N. Engl. J. Med | 37 centersɸ | 626 | 626 | 5 | 5 | ||||
| Ballard et al | April, 2004 | 2000. 11-2003. 5 | USA | J. Vasc. Surg. | single-center | 22 | 107 | PNR | … | … | PCS-12 and MCS-12ɸ |
| Elkouri et al | March, 2004 | 1999. 12. 1-2001. 12. 1 | USA | J. Vasc. Surg. | single-center | 94 | 261 | Retro. | > 0.08 | > 0.08 | |
| Lee et al | March, 2004 | 2001. 1. 1-2001. 12. 31 | USA | J. Vasc.Surg. | 986 hospitals | 2565 | 4607 | Retro. | … | … | |
| Zeebregts et al | January, 2004 | 1998. 4-2003. 1 | Netherlands | Brit. J. Surg. | single-center | 93 | 82 | PNR | 1.6 | 1.7 | Exclude former OSR |
| Moore et al | July, 2003 | 1995. 11. 22-1998. 2. 12 | USA | J. Vasc. Surg. | multicenter | 573 | 111 | PNR | 5 | 5 | EGS & Ancure £ |
| Jordan et al | May, 2003 | 2000. 1. 1-2002. 6. 12 | USA | Ann. Surg. | single-center | 130 | 87 | Retro. | … | … | High-Risk |
| Criado et al | April, 2003 | 1999. 3. 24-2000. 9. 19 | USA | J. Vasc. Surg. | 17 centers | 240 | 126 | PNR | 1.1 | 0.9 | Talent LPS |
| Matsumura et al | February, 2003 | 1998. 12-2000. 1 | USA | J. Vasc. Surg. | 19 centers | 235 | 99 | PNR | 5 | 5 | Excluder |
| Peterson et al | May, 2007 | ||||||||||
| Hansman et al | January, 2003 | 1999. 11 - 2002. 1 | USA | Am. J. Surg. | single-center | 50 | 50 | Retro. | … | … | |
| Arko et al | 2003 | 1996. 10-2000. 7 | USA | J. Endovasc. Ther. | single-center | 153 | 141 | Retro. | … | … | |
| Ligush et al | September, 2002 | 1999. 12-2001. 6 | USA | J. Vasc. Surg. | single-center | 33 | 66 | Retro. | … | … | |
| Teufelsbauer et al | July 29, 2002 | 1995. 1-2000. 12 | Austria | Circulation. | single-center | 206 | 248 | Retro. | 2.5 | 2.5 | |
| Cuypers et al | April 15, 2001 | 1996. 9-1999. 10 | Netherlands | Brit. J. Surg. | 2 centers | 57 | 19 | RCT | … | … | |
| Brewster et al | June, 1998 | 1994. 1-1997. 5 | USA | J. Vasc. Surg. | single-center | 28 | 28 | Retro. | … | … |
Note:EVAR: elective endovascular repair; OSR: elective open surgical repair;Retro: retrospective data collection; PNR: prospective non-randomized trial;RCT: randomized controlled trial;
$: Database described as Canadian Institute for Health Information Discharge Abstract Database in Ontario
£: Stents system described as Talent enhanced Low Profile System
†: Database described as Vascular Study Group of Northern New England, in this paper we excluded the following data: Carotid endarterectomy, lower extremity bypass and rupture AAA open surgical repair.
‖: Database described as Veterans Health Administration’s National Surgical Quality Improvement Program.
‡: The following endografts were used: Guidant-AnCure, Medtronic-AneuRx, Gore-Excluder and Endologix-PowerLink.
¶: Database described as National Surgical Quality Improvement Program Private Sector.
§: The composition of the DREAM Trial Group includes 24 centers in the Netherlands and 4 centers in Belgium.
ɸ: Until August 2004, the EVAR trial consisted of 37 clinical centers which included 34 centers that were reported in 2004 and 2005 and an additional 3 centers that contributed 170 patients.
ɸ: Two scoring systems were considered: PCS, Physical Component Summary score and MCS, Mental Component Summary score.
£: Stents system includes an EGS component at 18 sites and an Ancure component at 21 sites.
The twenty-one Chinese language papers contained 1,405 AAA procedures. The Chinese language articles were published between 1993 and 2010 (Table 2).
| Study | Month and Year of Publication | Study Period | Total | Actual | EVAR | OSR | Follow-up EVAR | Follow-up OSR | Database |
|---|---|---|---|---|---|---|---|---|---|
| LI Honghao et al | September, 2010 | 2001.1. 1-2008. 12. 31 | 33 | 27 | 11 | 16 | … | … | Sun Yat-sen Memorial Hospital |
| LI Xinxi et al | June, 2010 | 2002-2008 | 58 | 58 | 25 | 33 | … | … | The First Affiliated Hospital of Xinjiang Medical University |
| Lu Shengwei et al | June, 2010 | 2005.6-2009. 3 | 62 | 62 | 29 | 33 | 1.5 | 1.5 | The First Affiliated Hospital of Guangxi Medical University |
| Meng Fanxin et al | June, 2010 | 1999.1. 1-2010. 1. 1 | 92 | 53$ | 28 | 25 | 3 | 3.3 | Peking Union Medical College Hospital |
| Yue Wenliang et al | May, 2010 | 2004.1-2009. 4 | 112 | 112 | 66 | 46 | … | … | The First Affiliated Hospital of China Medical University |
| Qiu Jian et al | May, 2010 | 2003-2010 | 120 | 120 | 36 | 84 | £ | £ | The Second Xiangya Hospital, Central South University |
| Jiang Lanshan et al | March, 2010 | 2004-2009 | 23 | 23 | 6 | 17 | < 2 | < 6 | Mian yang Central Hospital |
| Zhang Jinglan et al | 2010 | NG | 90 | 90 | 44 | 46 | … | … | Beijing Anzhen Hospital, Capital Medical University |
| Ding Hao et al§ | October, 2009 | 2000.1. 1-2008. 12. 31 | 30 | 30 | 8 | 22 | 1 | 1 | The First Affiliated Hospital of Anhui Medical University |
| Chen Weiqing et al§ | August, 2009 | 2001.6-2008. 1 | 31 | 23 | 4 | 19 | 3.2 | 3.2 | Tianjin Medical University General Hospital |
| Zhang Yongjie et al§ | June, 2009 | 2002.1-2007. 7 | 42 | 42 | 12 | 30 | 2.7 | 2.7 | Central Hospital City of Zibo |
| Chen Yushuai et al§ | December, 2008 | 2000.7-2005. 12 | 54 | 54 | 20 | 34 | 2.7 | 2.7 | First Affiliated Hospital of China Medical University |
| Tang Xiaobin et al | September, 2008 | 2001.1-2007. 7 | 223 | 223 | 82 | 141 | 2.7 | 2.7 | Beijing Anzhen Hospital, Capital Medical University |
| Ye Jinming et al | September, 2008 | 2005.2-2007. 6 | 75 | 72 | 49 | 23 | … | … | Zhejiang Hospital & Zhongshan Hospital,Fudan University |
| Du Qingguo et al | 2007 | 2002.2-2006. 2 | 37 | 37 | 14 | 23 | … | … | The First Affiliated Hospital, Chongqing Medical University |
| Yao Chen et al | January, 2006 | 2003.10-2004. 10 | 34 | 34 | 15 | 19 | 0.9 | 0.9 | The First Affiliated Hospital, Sun Yat-sen University |
| Dong Yifei et al | December, 2005 | 2003.1-2005. 4 | 23 | 23 | 3 | 20 | … | … | Lanzhou General Hospital, Lanzhou Command, PLA |
| Shu Chang et al | June, 2003 | 1999-2002 | 26 | 21 | 7 | 14 | … | … | The Second Xiangya Hospital, Central South University |
| Feng Rui et al† | February, 2003 | 1997.3-2002. 3 | 157 | 157 | 115 | 42 | … | … | Changhai Hospital, Second Military Medical University |
| Fu Weiguo et al | 2003 | 1998.9-2001. 10 | 92 | 92 | 31 | 61 | 2 | 2 | Zhongshan Hospital, Fudan University |
| Guo Wei et al | June, 2000 | 1993.6-1999. 8 | 52 | 52 | 20 | 32 | … | … | General Hospital, People's Liberation Army (PLA) |
Note:
$: There were 92 patients involved with sufficient reported data. However only 53 had follow-up data, which we included in our analysis.
£: Although the study reported the survival curve, sufficient data was not reported.
§: Despite mean follow-up time being given the studies did not provide a detailed number for death or survival.
†: This study mainly discussed EVAR and OSR affecting renal function.
Within the Western papers, a total of 31,074 elective AAA procedures were reported, of which 12,774 were EVAR and 18,300 were OSR. By comparison, a total of 1,405 operations were performed for unruptured AAA in the Chinese papers, of which 625 were EVAR and 780 were OSR. There are significant difference across racial groups, with Chinese patients more likely to receive EVAR compared to Western patients (P = 0.012) (Table 3).
| Racial/ethnic group | EVAR (N = 13,399) | OSR (N = 19.080) | Total (N = 32,479) |
|---|---|---|---|
| Western population | 12,774 (41.1%) | 18,300 (58.9%) | 31,074 |
| Chinese population | 625 (44.5%) | 780 (55.5%) | 1,405 |
Note: EVAR: elective endovascular repair; OSR: elective open surgical repair;
Table 4 shows that four RCT studies adequately performed all methodological requirements as assessed by the Cochrane risk of bias tool and Jadad’s scoring system, and three were considered to be at low risk of bias, with the remaining trial was graded at moderate risk. Furthermore, for Western non-randomized studies, 19 (21 papers) of 34 studies (37 papers) achieved an ideal score of 24 points. However, 15 studies did not report follow-up data and therefore did not meet the criterion for the item “loss of follow-up less than 5%” and were thus allotted 22 points.
| Study | Year of Publication | EVAR | OSR | Cochrane Reviewer’s Handbook | Jadad | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adequate sequence generation | Allocation concealment | Blinding | Withdrawals and drop outs | ITT | Risk of bias | Randomization | Double blinding | Withdrawals and drop outs | Jadad’s score | ||||
| Soulez et al | August,2005 | 20 | 20 | computer | met | unclear | unmet | unclear | B | 2 | 1 | 0 | 3 |
| DREAM | October,2004 |
171 | 174 | computer | met | double blinding | met | met | A | 2 | 2 | 1 | 5 |
| EVAR-1 | August,2004 |
543 | 539 | computer | met | double blinding | met | met | A | 2 | 2 | 1 | 5 |
| Cuypers et al | April,2001 | 57 | 19 | computer | met | double blinding | met | met | A | 2 | 2 | 1 | 5 |
Note: ITT (intent-to-treat)
Patient characteristics:
In Table 5 we provide the demographic and clinical characteristics of all the patients included in this review, broken down by treatment group. A significant difference was present for sex in Western cohorts, with more male patients in the EVAR group (OR = 1.692, P < 0.001) whereas this difference was not present in Chinese cohorts (OR = 1.007, P = 0.972). Whether Western or Chinese, patients in the EVAR group were significantly older than those in the OSR group (P < 0.001 and P = 0.008), nevertheless, the age range was larger in Chinese cohorts (WMDWestern 2.413 years versus WMDChinese 3.63 years). The maximum diameter of the aneurysms in the EVAR group was significantly smaller than in the OSR group for both cohorts (P < 0.001 and P < 0.001). Also, the range was larger for the Chinese cohorts than for the Western cohorts (WMDWestern -2.491 mm versus WMDChinese -5.793 mm).
| Characteristic | Region | No. of studies | EVAR | OSR | OR/WMD | 95% CI | Weight | P | ||
|---|---|---|---|---|---|---|---|---|---|---|
| n (%)* | N | n (%)* | N | |||||||
| Male Gender-No. | Chinese | 10 | 338 (86.2) | 392 | 411 (83.7) | 491 | 1.007 | 0.678,1.497 | 9.25 | 0.972 |
| Western | 34 | 10,870 (87.7) | 12,290 | 14,708 (81.9) | 17,954 | 1.692 | 1.460,1.961 | 90.75 | < 0.001 | |
| Total | 44 | 11,208 (88.4) | 12,682 | 15,119 (82.0) | 18,445 | 1.614 | 1.408,1.849 | 100.00 | < 0.001 | |
| Mean age-Year¶ | Chinese | 11 | 67.31 | 313 | 63.69 | 433 | 3.630 | 0.959,6.302 | 10.50 | 0.008 |
| Western | 19 | 73.33 | 8,399 | 70.68 | 8,541 | 2.413 | 1.845,2.982 | 89.50 | < 0.001 | |
| Total | 30 | 70.32 | 8,712 | 67.19 | 8,974 | 2.555 | 2.007,3.103 | 100.00 | < 0.001 | |
| Hypertension-No. | Chinese | 12 | 209 (51.7) | 404 | 327 (56.9) | 575 | 1.139 | 0.711,1.826 | 14.85 | 0.588 |
| Western | 28 | 7,127 (67.3) | 10,593 | 10,091 (63.3) | 15,934 | 1.096 | 0.961,1.251 | 85.15 | 0.170 | |
| Total | 40 | 7,336 (66.7) | 10,997 | 10,418 (63.1) | 16,509 | 1.098 | 0.966,1.249 | 100.00 | 0.153 | |
| Hyperlipidemia -No. | Western | 14 | 1,169 (46.1) | 2,534 | 1,459 (43.8) | 3,333 | 1.213 | 0.928,1.587 | 100.00 | 0.158 |
| Diabetes Mellitus-No. | Chinese | 10 | 57 (14.4) | 395 | 55 (10.8) | 510 | 1.364 | 0.899,2.070 | 12.44 | 0.144 |
| Western | 29 | 1,533 (14.4) | 10,658 | 2,244 (13.9) | 16,123 | 1.248 | 1.028,1.514 | 87.56 | 0.025 | |
| Total | 39 | 1,590 (14.4) | 11,053 | 2,299 (13.8) | 16,633 | 1.266 | 1.063,1.507 | 100.00 | 0.008 | |
| Cardiac Disease-No. | ChineseΔ | 8 | 136 (42.1) | 323 | 122 (35.0) | 349 | 1.404 | 0.799,2.466 | 13.58 | 0.238 |
| Western† | 24 | 3,923 (47.3) | 8,301 | 2,485 (28.2) | 8,807 | 1.137 | 0.899,1.438 | 57.94 | 0.283 | |
| Western§ | 13 | 902 (14.1) | 6,390 | 622 (6.3) | 9,820 | 2.901 | 1.995,4.218 | 28.48 | < 0.001 | |
| Total$ | NC | NC | NC | NC | NC | 1.522 | 1.236,1.873 | 100.00 | < 0.001 | |
| Pulmonary Disease-No. £ | Chinese | 6 | 41 (17.2) | 239 | 50 (18.2) | 274 | 1.069 | 0.661,1.728 | 10.90 | 0.787 |
| Western | 26 | 3,448 (33.0) | 10,438 | 3,997 (25.6) | 15,642 | 1.515 | 1.209,1.899 | 89.10 | < 0.001 | |
| Total | 32 | 3,489 (32.7) | 10,677 | 4,047 (25.4) | 15,916 | 1.458 | 1.182,1.799 | 100.00 | < 0.001 | |
| Renal Disease-No.ɸ | Chinese | 4 | 10 (5.8) | 172 | 10 (6.6) | 152 | 1.041 | 0.352,3.074 | 6.65 | 0.942 |
| Western | 18 | 564 (6.1) | 9,283 | 833 (5.8) | 14,280 | 1.270 | 0.902,1.789 | 93.35 | 0.171 | |
| Total | 22 | 574 (6.1) | 9,455 | 843 (5.8) | 14,432 | 1.251 | 0.903,1.733 | 100.00 | 0.178 | |
| Cerebrovascular Disease-No. | Chinese | 5 | 25 (11.4) | 220 | 23 (7.4) | 311 | 1.726 | 0.626,4.762 | 10.21 | 0.292 |
| Western | 12 | 361 (6.6) | 5,477 | 731 (6.1) | 12,014 | 1.287 | 1.091,1.517 | 89.79 | 0.003 | |
| Total | 17 | 386 (6.8) | 5,697 | 754 (6.1) | 12,325 | 1.258 | 1.019,1.553 | 100.00 | 0.033 | |
| Smoking-No. ‡ | Chinese | 7 | 71 (45.8) | 155 | 152 (53.5) | 284 | 0.723 | 0.473,1.106 | 16.64 | 0.135 |
| Western | 21 | 3,145 (70.4) | 4,465 | 2,950 (64.5) | 4,571 | 1.057 | 0.813,1.375 | 83.36 | 0.677 | |
| Total | 28 | 3,216 (69.6) | 4,620 | 3,102 (63.9) | 4,855 | 0.999 | 0.793,1.258 | 100.00 | 0.992 | |
| Peripheral Vascular Disease-No. | Chinese | 6 | 77 (28.9) | 266 | 73 (24.3) | 300 | 0.788 | 0.496,1.251 | 24.21 | 0.312 |
| Western | 10 | 1,005 (19.5) | 5,162 | 2,576 (22.4) | 11,493 | 1.163 | 0.764,1.771 | 75.79 | 0.482 | |
| Total | 16 | 1,082 (19.9) | 5,428 | 2,649 (22.5) | 11,793 | 1.057 | 0.742,1.505 | 100.00 | 0.760 | |
| Aneurysm Diameter-mm¶ | Chinese | 10 | 54.31 | 247 | 60.31 | 387 | -5.793 | (-7.993,-3.594) | 13.69 | < 0.001 |
| Western | 15 | 57.71 | 4,790 | 60.41 | 2,768 | -2.491 | (-3.307,-1.675) | 86.31 | < 0.001 | |
| Total | 25 | 56.01 | 5,037 | 60.36 | 3,155 | -2.932 | (-3.697,-2.168) | 100.00 | < 0.001 | |
| ASA>Ⅱ-No. ǂ | Western | 9 | 1,783 (74.4) | 2,395 | 1,646 (67.4) | 2,441 | 2.637 | 1.307,5.322 | 100.00 | 0.007 |
Note: *: The number of patients for dichotomous data (values in parentheses are percentages) and average for continuous data. NC: not calculated.
OR: odds radio. WMD: weighted mean difference. CI: confidence interval.
¶: Outcomes presented as weighted mean difference.
Δ: Reported in studies as coronary artery disease/ischaemic heart disease from Chinese studies.
†: Reported in studies as coronary artery disease/ischaemic heart disease from Western studies.
§: Reported in studies as congestive heart failure from Western studies.
$: Not calculated because a portion of the total number of patients with cardiac disease combined both CAD and CHF.
£: Reported in studies as chronic obstructive pulmonary disease/ pulmonary disease.
ɸ: Reported in studies as renal failure/renal insufficiency/renal dysfunction.
‡: Reported in studies as smoking present/history of smoking.
ǂ: Denotes American Society of Anesthesiologists, the total scores more than Ⅱ
P values in bold denote statistical significance.
We found that the EVAR group had a higher rate of co-morbid conditions in Western studies, with a statistically significant difference in three of the baseline medical conditions; these were diabetes mellitus (OR = 1.248, P = 0.025), respiratory disease (OR = 1.515, P < 0.001) and cerebrovascular disease (OR = 1.287, P = 0.003). However, these differences were not present in the Chinese cohort. In addition, Western patients with the American Society of Anesthesiologists classification III or IV were more likely to receive elective EVAR than OSR (OR = 2.637, P = 0.007). Of note, thirteen Western studies showed a statistically significant difference in the odds ratio (OR = 2.901, P < 0.001) for congestive heart failure between the EVAR group and OSR group. No significant difference, however, was found in other aspects of cardiac disease in the Western and Chinese cohorts.
Characteristics for surgical and post-operative data are given in Table 6. Information on the type of anesthesia was available for seven Western studies: 36.1 percent of 1,612 patients receiving endovascular repair received a general anesthetic compared with 94.3 percent of 1,393 patients receiving open surgical repair (OR = 0.055, P < 0.001). Most of the surgical characteristics showed significant differences between the EVAR and OSR groups both for Chinese and Western cohorts. The duration of a typical EVAR procedure (mean 183.8 minutes versus 149.9 minutes) was significantly different than that of a typical OSR procedure (mean 261.9 versus 184.1 minutes) (WMDChinese -82.2 minutes versus WMDWestern -33.6 minutes, P < 0.001 versus P < 0.001, respectively).
| Characteristic | Region | No. of studies | EVAR | OSR | OR/WMD | 95% CI | Weight | P | ||
|---|---|---|---|---|---|---|---|---|---|---|
| n | N | N | N | |||||||
| General anaesthetic-No. | Western | 7 | 582 (36.1) | 1,612 | 1313 (94.3) | 1,393 | 0.055 | 0.014, 0.216 | 100.00 | < 0.001 |
| Operative time-min. | Chinese | 15 | 183.8 | 416 | 261.9 | 601 | -82.192 | (-101.793, -62.590) | 45.88 | < 0.001 |
| Western | 14 | 149.9 | 3,395 | 184.1 | 8,127 | -33.557 | (-45.179, -21.935) | 54.12 | < 0.001 | |
| Total | 29 | 166.9 | 3,811 | 223.0 | 8,728 | -56.659 | (-67.483, -45.836) | 100.00 | < 0.001 | |
| Blood Loss-ml. | Chinese | 15 | 156.8 | 416 | 965.3 | 601 | -640.454 | (-751.134, -529.774) | 54.23 | < 0.001 |
| Western | 13 | 341.6 | 1,820 | 1463.5 | 1,937 | -989.139 | (-1.2e+0.3, -828.958) | 45.77 | < 0.001 | |
| Total | 28 | 249.2 | 2,236 | 1214.4 | 2,538 | -829.134 | (-952.542, -705.726) | 100.00 | < 0.001 | |
| Blood Transfusion-ml. | Chinese | 13 | 52.3 | 388 | 694.5 | 547 | -517.31 | (-595.507, -439.112 | 75.50 | < 0.001 |
| Western | 4 | 70.1 | 784 | 383.0 | 783 | -312.695 | (-62.053, -3.337) | 24.50 | 0.048 | |
| Total | 17 | 61.2 | 1,172 | 538.8 | 1,330 | -471.091 | (-541.958, -400.223) | 100.00 | < 0.001 | |
| ICU Stay-hr | Chinese | 11 | 31.1 | 275 | 64.3 | 330 | -29.397 | (-37.048, -21.747) | 47.57 | < 0.001 |
| Western | 13 | 16.7 | 3,697 | 75.5 | 8,472 | -52.785 | (-65.280, -40.290) | 52.43 | < 0.001 | |
| Total | 24 | 23.9 | 3,972 | 69.9 | 8,802 | -42.479 | (-51.105, -33.853) | 100.00 | < 0.001 | |
| Postoperative Stay-days | Chinese | 11 | 11.1 | 256 | 14.9 | 387 | -4.179 | (-5.828, -2.531) | 46.96 | < 0.001 |
| Western | 6 | 3.9 | 2,063 | 8.4 | 2,602 | -4.556 | (-5.469, -3.643) | 53.04 | < 0.001 | |
| Total | 17 | 7.5 | 2,319 | 11.7 | 2,989 | -4.457 | (-5.140, -3.773) | 100.00 | < 0.001 | |
| Length of Stay-days | Chinese | 5 | 24.0 | 199 | 26.5 | 234 | -2.680 | (-5.182, -0.178) | 10.80 | 0.036 |
| Western | 6 | 4.8 | 5,175 | 10.6 | 7,018 | -5.608 | (-6.176, -5.039) | 89.20 | < 0.001 | |
| Total | 11 | 14.4 | 5,374 | 18.6 | 7,252 | -5.300 | (-5.850, -4.750) | 100.00 | < 0.001 | |
Note: ICU stay: intensive care unit.
Considering either the volume of blood loss or blood transfusion, the superiority of endovascular repair over open surgical repair was clear. Specifically, in the Western cohort the range of blood loss between EVAR and OSR was even larger (WMDWestern -989.1 ml versus WMDChinese -640.5 ml). Nevertheless, the range of blood transfusion between the two procedures was even smaller (WMDWestern -312.7 ml versus WMDChinese -517.3 ml), namely, contract by OSR, Chinese patients undergoing EVAR were transfused less blood (approximately a unit) than Western patients.
In addition, patients who underwent EVAR experienced significantly shorter stays in the intensive care unit (ICU) and the hospital for both Western and Chinese cohorts. The Western patients who underwent EVAR had significantly shorter stays in the ICU (WMDWestern -52.785 hours, P < 0.001) and significantly shorter duration in the hospital (WMDWestern -5.608 days, P < 0.001) than Chinese patients.
Table 7 presents a more detailed overview of the reported complications; the Western pooled estimate of the cardiac complication rate for EVAR was significantly lower than that for OSR (ORWestern = 0.411, P < 0.001). This superiority for EVAR was not replicated in the Chinese cohorts, however. Whether in Chinese or Western cohorts, endovascular repair was associated with a significant reduction in postoperative respiratory complications, however, the Chinese complication rate for the respiratory system (OR = 0.270, P < 0.001) in the EVAR group was lower than in Western patients (OR=0.552, P = 0.029) receiving EVAR. There was no significant difference in the incidence of renal, cerebrovascular, and wound complications. Furthermore, Chinese limb ischaemia or embolization were more common (ORChinese = 1.539, P = 0.049) in patients receiving EVAR, although Western studies did not contain this difference. In addition, the pooled estimate of 30-day mortality in Western studies for the EVAR group was significantly lower than that for the OSR group (OR = 0.481, P < 0.001), however this difference was not present in the Chinese cohort (OR = 0.733, P = 0.425) (Fig. 3).
| Characteristic | Region | No. of studies | EVAR | OSR | OR | 95% CI | Weight | P | ||
|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | N | n (%) | N | |||||||
| Cardiac Complications-No. | Chinese | 13 | 20 (5.2) | 382 | 55 (9.8) | 563 | 0.683 | 0.405,1.153 | 9.15 | 0.154 |
| Western | 19 | 240 (3.7) | 6,437 | 642 (7.3) | 8,852 | 0.411 | 0.348,0.485 | 90.85 | < 0.001 | |
| Total | 32 | 260 (3.8) | 6,819 | 697 (7.4) | 9,415 | 0.430 | 0.367,0.504 | 100.00 | < 0.001 | |
| Pulmonary Complications-No. | Chinese | 15 | 17 (3.9) | 435 | 60 (9.3) | 646 | 0.552 | 0.324,0.940 | 11.58 | 0.029 |
| Western | 18 | 152 (3.4) | 4,427 | 573 (11.4) | 5,044 | 0.270 | 0.222,0.328 | 88.42 | < 0.001 | |
| Total | 33 | 169 (3.5) | 4,862 | 633 (11.1) | 5,690 | 0.293 | 0.245,0.352 | 100.00 | < 0.001 | |
| Renal Complications-No. | Chinese | 9 | 12 (3.5) | 341 | 21 (4.5) | 468 | 0.740 | 0.336,1.631 | 11.82 | 0.455 |
| Western | 19 | 529 (5.8) | 9,056 | 747 (7.8) | 9,617 | 1.081 | 0.765,1.529 | 88.18 | 0.659 | |
| Total | 28 | 541 (5.8) | 9,397 | 768 (7.6) | 10,085 | 1.029 | 0.752,1.408 | 100.00 | 0.859 | |
| Cerebrovascular Complications-No. | Chinese | 4 | 3 (1.9) | 158 | 7 (3.2) | 216 | 1.011 | 0.223,4.588 | 10.52 | 0.988 |
| Western | 11 | 31 (0.9) | 3,183 | 39 (1.3) | 3,113 | 0.836 | 0.508,1.374 | 89.48 | 0.479 | |
| Total | 15 | 34 (1.0) | 3,341 | 46 (1.4) | 3,329 | 0.854 | 0.534,1.367 | 100.00 | 0.511 | |
| Wound Complications-No. | Chinese | 9 | 9 (2.3) | 388 | 24 (5.0) | 481 | 0.743 | 0.353,1.564 | 25.48 | 0.433 |
| Western | 16 | 148 (4.1) | 3,617 | 384 (10.0) | 3,856 | 0.720 | 0.357,1.453 | 74.52 | 0.359 | |
| Total | 25 | 157 (3.9) | 4,005 | 408 (9.4) | 4,337 | 0.686 | 0.390,1.208 | 100.00 | 0.192 | |
| Limb ischaemia/ embolization-No. | Chinese | 8 | 11 (4.4) | 251 | 7 (1.8) | 396 | 1.539 | 1.004,3.198 | 26.23 | 0.049 |
| Western | 8 | 50 (2.5) | 1,979 | 52 (2.5) | 2,075 | 0.914 | 0.462,1.809 | 73.77 | 0.796 | |
| Total | 16 | 61 (2.7) | 2,230 | 59 (2.4) | 2,471 | 1.106 | 0.923,1.303 | 100.00 | 0.410 | |
| Re-intervention-No. | Western | 6 | 188 (13.4) | 1,401 | 103 (6.5) | 1,581 | 1.962 | 0.932,4.176 | 100.00 | 0.080 |
| 30 day mortality-No. | Chinese | 12 | 8 (2.3) | 352 | 22 (4.1) | 542 | 0.733 | 0.342,1.572 | 7.04 | 0.425 |
| Western | 33 | 218 (1.8) | 12,133 | 674 (3.8) | 17,817 | 0.481 | 0.378,0.612 | 92.96 | < 0.001 | |
| Total | 45 | 226 (1.8) | 12,485 | 696 (3.8) | 18,359 | 0.490 | 0.399,0.602 | 100.00 | < 0.001 | |
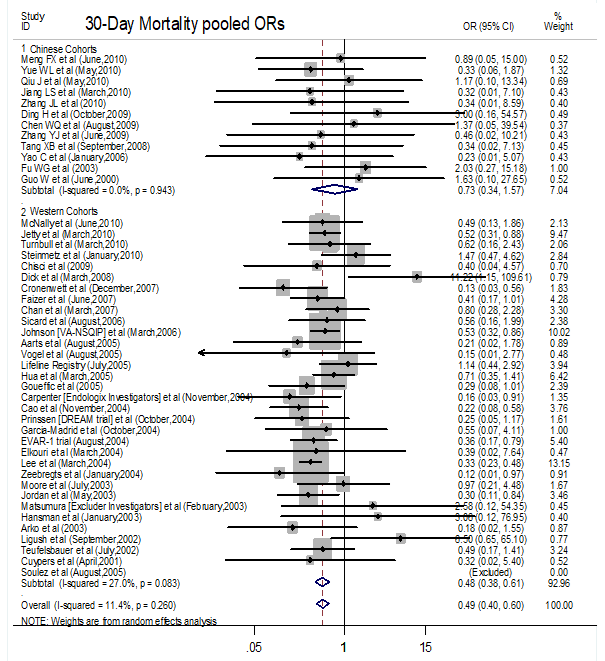 Figure 3.
Figure 3.Forest plot of 30-day mortality following endovascular aortic aneurysm repair (EVAR) or open surgery repair (OSR) to the treatment of elective abdominal aortic aneurysms (AAAs) between China and Western countries.
3.8.1 Pooled ORs for Western studies
In Western countries the amount of medium-long term research in this field is far more than in China and it is therefore far easier to reach a satisfactory outcome using Western studies. Consequently, we have primarily based the analysis of the mid-long term comparison of the two AAA treatment methods on Western studies.
Fifteen, four, and nine articles reported data for all-cause mortality at one year, two-three years and more than five years, respectively. In an analysis of the pooled data we found no significant difference in all-cause mortality at one year, 2-3 years and more than five years (OR = 0.932, 95% CI: 0.723-1.203; P = 0.590 for one year) (OR = 0.850, 95% CI: 0.407-1.774; P = 0.665 for 2-3 years) (OR = 1.301, 95% CI: 0.982-1.724; P = 0.067 for more than 5 years) respectively (Fig. 4).
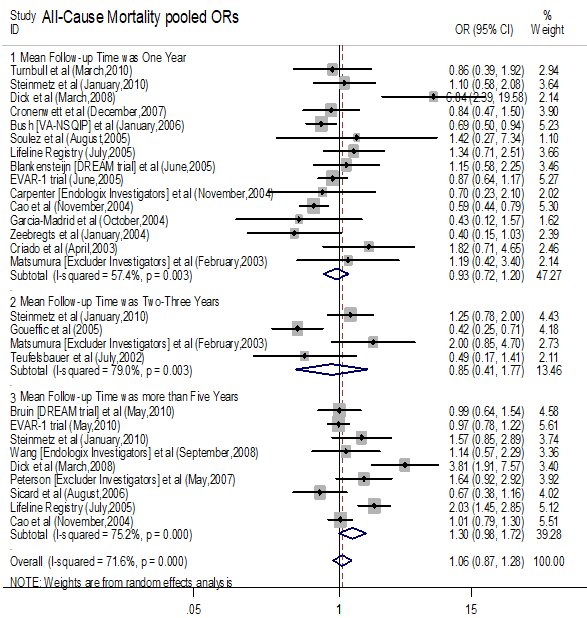 Figure 4.
Figure 4.Forest plot of all cause mortality following endovascular aortic aneurysm repair (EVAR) or open surgery repair (OSR) during follow-up time at one year, 2-3 years and more than five years after discharge.
Eight and three articles, respectively, compared aneurysm-related mortality for medium term aneurysm-related mortality and more than 5 years between endovascular repair group and open surgery groups, which showed that medium-term (mean follow-up time was 2-3 years) aneurysm-related mortality (OR = 0.566, 0.402-0.796; P = 0.001) was significantly lower after EVAR compared to OSR. Endovascular repair did not, however, influence long-term (mean follow-up time was more than five years) aneurysm-related mortality (OR = 0.639, 95% CI: 0.360-1.133; P = 0.125) (Fig. 5).
 Figure 5.
Figure 5.Forest plot of aneurysm-related mortality following endovascular aortic aneurysm repair (EVAR) or open surgery repair (OSR) during follow-up time at 2-3 years and more than five years after discharge.
An analysis of eight studies with 1-year follow-up data showed that patients receiving EVAR were more likely to experience re-intervention, (OR = 2.042, 95 % CI: 1.467-2.843; P < 0.001) compared to OSR patients. Additionally, an analysis of four studies involving 3,214 participants with 3-year follow-up data showed that EVAR patients were more likely to experience re-intervention (OR = 4.107, 95% CI: 2.304-7.318; P < 0.001) than OSR patients (Fig. 6).
 Figure 6.
Figure 6.Forest plot of rate of re-intervention following endovascular aortic aneurysm repair (EVAR) or open surgery repair (OSR) during follow-up time at one years and more than three years after discharge.
3.8.2 Pooled HRs for Western and Chinese studies
Although there were few studies reporting aneurysm-related mortality and the rate of re-intervention, we included the three Chinese articles which reported all-cause mortality (Fig. 7). These studies had a mean follow-up time of 25.4 to 37.6 months and involved 265 participants (95 in EVAR, 170 in OSR). The medium-long term all-cause mortality to a maximum follow-up period of 4 years was not significantly higher (HR = 1.173, 95% CI: 0.895-1.538; P = 0.247) for the EVAR group than the OSR group.
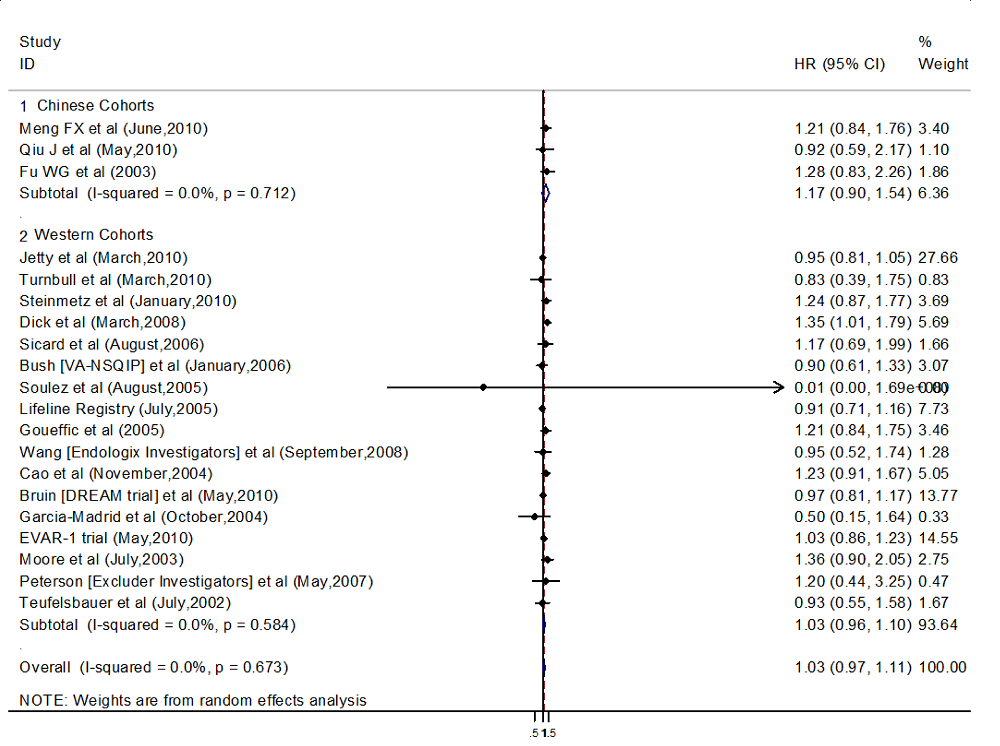 Figure 7.
Figure 7.Forest plot of all-caused mortality pooled HR (hazard ratio) following endovascular aortic aneurysm repair (EVAR) or open surgery repair (OSR) during follow-up time.
Data on all-cause mortality were reported in seventeen trials from Western studies. These studies included 9,994 participants, with a mean follow-up time ranging from 19.2 to 76.8 months. We found no statistically significant difference in the risk of all-cause mortality between the EVAR and OSR patients (HR = 1.026, 95% CI: 0.956-1.100; P = 0.483).
Publication bias was evaluated with a funnel plot of all analyses reporting on 30-day mortality following elective abdominal aortic aneurysm repair. all the points were within the trilateral region (Fig. 8A). Furthermore, publication bias was evaluated using the Begg test (result: P = 0.122) and Egger test (result: P > |t| was 0.920), and the Egger linear regression asymmetry plot frequently tended to show the presence of publication bias (Fig. 8B). The plot displays that the regression line passes through the point of origin, which may indicate the absence of bias.
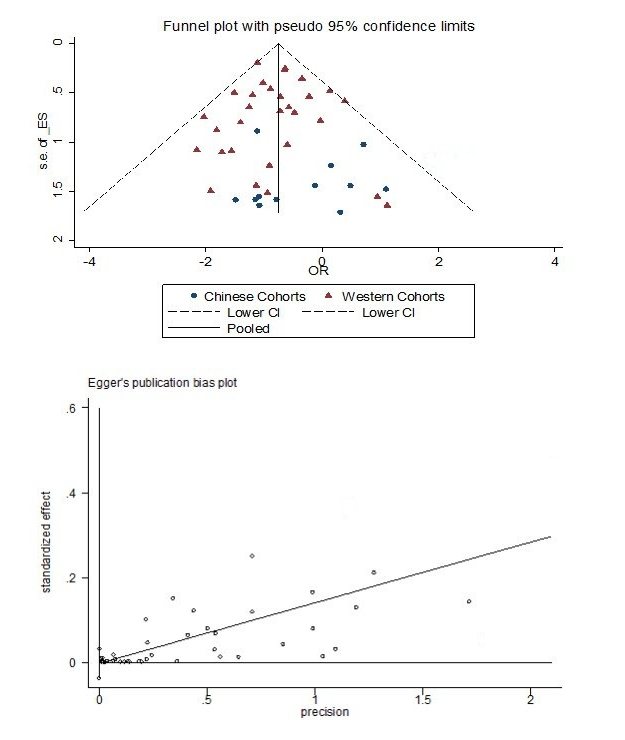 Figure 8.
Figure 8.a. The funnel plot to assess publication bias from 30-day mortality data from Chinese and Western studies. b. Egger’s publication bias plot to assess publication bias from 30-day mortality data from Chinese and Western studies.
Patient racial and ethnic variations reflect racial disparities in socioeconomic status and patient-level differences (Chen et al., 2006). The use of different providers (Baicker et al., 2005; Byrd and Clayton, 2002; Bach et al., 2004) and different treatment by the same provider (Schulman et al., 1999) have been shown to result in disparate practice patterns and outcomes depending on race and ethnicity. Additionally, race and ethnicity have been shown to predict disparities, treatment variations and postoperative outcomes in the surgical arena (Jha et al., 2005; Epstein et al., 2010; Andrew et al., 2000). Less is known about racial/ethnic differences in cardiovascular procedure outcomes. Although large and multiregional cohort studies have shown that minority patients such as black and Hispanic patients are more likely to receive procedures in low-volume hospitals, these studies focus on diverse cardiovascular procedures for which there is a documented association between the disparities of ethnicity and hospital or surgeon volume (Epstein et al., 2010; Trivedi et al., 2006) Unfortunately, even though subsequent research has shown that racial and ethnic disparities account for differences of treatment in AAA, these studies were restricted to a specific racial comparison (black versus white or Hispanic versus white subjects).
Many studies (Lovegrove et al., 2008) assess the short- or mid-long term differences between EVAR and OSR and some of these studies reported on a large number of samples. Despite this, to the best of our knowledge, this is the first systematic review of the different outcomes due to ethnicity - specifically Western and Chinese - following EVAR or OSR for elective abdominal aortic aneurysms. Therefore, our study had some important strengths. This is the most (to our knowledge) comprehensive meta-analysis of patients treated for AAA, using a broad study sample captured through an electronic retrieval system. We used strict inclusion criteria and excluded patients with non-elective aneurysms (ruptured AAAs and inflammatory AAAs) because including them would adversely affect the analysis of the prognosis of patients, which would have distorted the study results. In addition, although heterogeneity is often a concern in meta-analyses, little evidence of heterogeneity was observed throughout our study. We performed a systematic search using multiple databases and extracted data in duplicate.
In this study we report the major differences between Chinese and Western cohorts in the treatment and outcomes of two major AAA procedures. We found a significantly low short-term respiration complication after EVAR Importantly, the examination of short-term outcomes confirmed that EVAR is associated with significantly low 30-day mortality in Western countries. The counterpart as well as China, nevertheless, EVAR has not exposed this superior. The racial/ethnic disparities we found can be partially explained by differences in the use of EVAR techniques, socioeconomic status and co-morbidities (Osborne et al., 2009). Additionally, several factors of providers (low-mortality, high-quality and high-volume hospitals) may be responsible for these differences in the outcomes of AAA procedures.
Chinese patients were more likely to receive EVAR (44%) compared to Western patients (41%). This difference in treatment may be due to four separate mechanisms First, these disparities could be attributed to confounding provider-patient factors such as decision making (Rathore and Krumholz, 2004) in provider care and differences in patient preferences (e.g., prevalence and morbidity of AAAs). Second, these disparities in treatment could be caused by anatomical differences in AAAs (e.g., EVAR suitability) between Chinese and Western patients. Third, these disparities could be caused by differences in the type and quantity of co-morbidities (e.g., cardiac and pulmonary morbidities with AAAs) that influence the treatment decision. Finally, objective factors due to socioeconomic status (e.g., insurance statues) may lead to the disparities in treatment. Patient mortality may be influenced by these disparities of treatment directly and indirectly. This study demonstrated a trend toward worse early outcomes of EVAR among Chinese subjects (30-day mortality was 2.3%) which is not significant diversity versus OSR.
A possible explanation for the disparity in AAA repair is patient preferences and provider-patient factors. Although little is known about the prevalence of AAAs among the racial and ethnic groups represented in this meta-analysis, two studies (Salem et al., 2009; Spark et al., 2001) have demonstrated a very low incidence of aneurysms in Asian subjects. This may provide some evidence to the prevalence of Chinese aneurysms. Unfortunately, their study was only a comparative research of the population confined to a specific geographical area (Leicester, Bradford in England). Perhaps Chinese patients will receive more medical attention for EVAR and therefore receive the minimally invasive procedure because of the lower prevalence of disease among Chinese patients compared to Western patients.
Anatomical variation may be responsible for racial disparities in the treatment and mortality of AAAs. Although most variation is unexplained by observable patients and provider factors, differences of ethnicity alone may be treated differently because of unmeasured factors such as anatomical variation and aneurysm size (Osborne et al., 2009). However, no previous studies to date have reported anatomical differences in AAAs between racial and ethnic groups, especially Chinese patients. Although there is no evidence available, through our analysis and previous work (Fu et al., 2003) it is plausible that Chinese patients may be predisposed to AAAs that are suitable for EVAR which may partially explain the disparity in treatment. A previous study (Osborne et al., 2009) suggested that the racial and ethnic disparity in mortality can be partially (29%) explained by differences in patient comorbidities. Therefore, this result also suggested that Chinese patients may have more challenging aortic anatomies (e.g., shorter common iliac arteries) and more access-related and device-related complications compared to Western patients (Wu et al., 2014; Tam et al., 2018).
A previous study (Osborne et al., 2009) also demonstrated that 26% of the disparity in mortality is due to differences in socioeconomic status. The type of insurance such as Medicare, Medicaid, private insurance and self-pay in American patients could partially represent differences in socioeconomic status. With regard to treatment disparities, they demonstrated that insurance status predicts disease severity at the time of treatment; however, after discharge, the outcomes are similar among insurance categories. Furthermore, uninsured and Medicaid patients possess different health statuses compared to Medicare and private insurance patients, which adversely influence peri-operative mortality. The Chinese literature does not clearly report the health insurance type and the expense of AAAs, but Asian patients were more likely to be enrolled in Medicare or uninsured, even though their socioeconomic status was higher than Black patients (Epstein et al., 2010).
Our study has a number of limitations. First, the method of reporting - including reporting of the frequency of events - was variable, making data aggregation challenging. Three studies have been adjusted systemically in the following fashion: (1) data from the same medical center has been reported by (Johnson et al., 2006; Bush et al., 2006) separately. Johnson reported the one-year follow-up data through 5 propensity groups, while Bush reported the survival analysis curve. Compared with Bush, Johnson provided a more complete analysis on the preoperative data. So we analyzed the preoperative data from Johnson's paper while using survival analysis results from Bush's paper. (2) (Carpenter and Endologix Investigators, 2004) published a paper in 2004 and Wang et al. (2008) published a paper in 2008 with both papers reporting the same outcome, but with different follow up times (Wang followed up as long as 81 months which was much longer than Carpenter). Therefore, we used Wang’s data to compute the HR value but used Carpenter's data to compute the OR value. (3) Although (Matsumura et al., 2003; Peterson et al., 2007) both reported their follow-up data, but we used Peterson's data to evaluate the long-term efficacy because of its different follow-up period and its analysis of survival data.
There were several other limitations. Our study data was limited to the available literature - although we used the VA (Veterans Affairs) and NIS (Nationwide Inpatient Sample) US databases, it would have been better to have had more available data. We couldn’t categorize the data according to racial/ethnic group. The Chinese literature data may include the Chinese population data. Our enrollment criterion was that both EVAR and OSR were reported in a comparative way; this made our Chinese sample much smaller than the Western sample. Additionally, Chinese papers published are much less than the Western literature. Finally, because this analysis was mainly based on data from Western and Chinese populations, additional investigation in other populations is still needed.
In conclusion, we found that Chinese patients were more likely to receive EVAR than OSR, and the post-procedure short-term mortality was significantly lower for EVAR than for OSR in Western patients but not in Chinese patients. Endovascular repair can be applied to Chinese patients with a reasonable safety margin. Further work is needed to explore the causes of these treatment differences.
Feng Shi and Yanshuo Han contributed to conception and design; Yuchen He, Yanshuo Han, Shiyue Wang and Jian Zhang contributed to acquisition of data, or analysis and interpretation of data; and Yanshuo Han and Chao Ji were involved in drafting the manuscript or revising it critically for important intellectual content. All authors have given final approval on the version to be published.
This work was supported by National Natural Science Foundation of China (grant number: 81600370), China Postdoctoral Science Foundation (grant number: 2018M640270) and Fundamental Research Funds for the Central Universities (grant number: DUT19RC(3)076) for Yanshuo Han, and Liaoning Provincial Natural Science Foundation of China (2019-ZD-0789) for Chao Ji.
We thank Ejear Editing Service (Ejear Editing Company) for editing the English text of a draft of the manuscript.
The authors declare no conflict of interest in preparing this article.
Pubmed
("Aortic Aneurysm, Abdominal"[Mesh] OR "AAA"[tiab] OR (("Aneurysm"[Mesh] OR "Aneurysm"[Tw] OR "Aneurysms"[Tw]) AND ("Abdomen"[Mesh] OR "Abdominal Cavity"[Mesh] OR "Abdomen"[Tw] OR "Abdominal"[Tw] OR "Aorta, Abdominal"[Mesh] OR (("Aorta"[Tw] OR "Aortic"[Tw]) AND ("abdominal"[tw] OR "abdomen"[tw]))))) AND ("Endovascular Procedures"[majr] OR "Endovascular"[ti] OR "EVAR"[ti] OR "eEVAR"[ti] OR "Minimal invasive"[ti] OR "Minimally-invasive"[ti] OR "Minimally invasive"[ti] OR "Stentgraft"[ti] OR "Stent-graft"[ti]) AND ("Open"[ti] OR "OSR"[ti] OR "OAR"[ti] OR "OR"[ti] OR "OS"[ti])
OVID
("Abdominal aorta aneurysm"/ OR "AAA".ti,ab. OR (("Aneurysm"/ OR "Aneurysm".mp. OR "Aneurysms".mp.) AND ("Abdomen"/ OR "Abdominal Cavity"/ OR "Abdomen".mp. OR "Abdominal".mp. OR "Abdominal aorta"/ OR (("Aorta".mp. OR "Aortic".mp.) AND ("abdominal".mp. OR "abdomen".mp.))))) AND (exp *"Endovascular surgery"/ OR "Endovascular".ti. OR "EVAR".ti. OR "eEVAR".ti. OR "Minimal invasive".ti. OR "Minimally-invasive".ti. OR "Minimally invasive".ti. OR "Stentgraft".ti. OR "Stent-graft".ti.) AND (*"open surgery"/ OR "Open".ti. OR "OSR".ti. OR "OAR".ti. OR "OR".ti. OR "OS".ti.)
Web of Science
TS = ("AAA" OR (("Aneurysm" OR "Aneurysms") AND ("Aorta" OR "Aortic") AND ("abdominal" OR "abdomen"))) AND TI = ("Endovascular" OR "EVAR" OR "eEVAR" OR "Minimal invasive" OR "Minimally-invasive" OR "Minimally invasive" OR "Stentgraft" OR "Stent-graft") AND TI = ("Open" OR "OSR" OR "OAR" OR "OR" OR "OS")
