Periodontitis is one of the risk factors associated with peripheral artery disease. This meta-analysis evaluates how periodontitis contributes to the pathogenesis and progression of peripheral artery disease. We systematically searched electronic databases Ovid Medline, Embase, Cochrane Library and Pubmed. Grey literature was also searched via Google Scholar. All studies evaluating the relationship between the incidence of periodontitis and peripheral artery disease were included. Subgroup analyses of carotid artery disease and lower extremity arterial disease were also conducted. Odds ratios (OR) and 95% confidence intervals (CI) were pooled and analyzed. The I 2 statistic was used to evaluate heterogeneity. Within a total of 25 studies, including 22,090 participants based on eligibility criteria, the incidence of peripheral artery disease was significantly higher among those with periodontitis (OR: 1.60, 95% CI 1.41-1.82, P < 0.001, I2 = 80.5%). In subgroup analysis, periodontitis was still a risk for lower extremity arterial disease (OR: 3.00, 95% CI 2.23-4.04, P < 0.001, I2 = 0%) and carotid artery disease (OR: 1.39, 95% CI 1.24-1.56, P < 0.001, I2 = 79.4%). Periodontitis is significantly associated with the incidence of lower extremity arterial disease and carotid artery disease.
Periodontitis is a chronic non-specific infectious disease which is prevalent worldwide (Eke et al., 2015). Tooth loss is a concomitant disease, occurring when chronic bacterial infection impacts periodontal support tissues. Australia's second National Adult Oral Survey (NSAOH) showed that mild periodontitis occurred among 20% of adults and that 1/40 suffered from it severely (Slade et al., 2004). Periodontitis is even worse among the indigenous population, 3/10 of whom suffer from severe periodontitis (Butten et al., 2019). Periodontitis may cause periodontal pocket formation, alveolar bone resorption, and tooth loosening, seriously affecting the quality of life of patients. Additionally, inflamed periodontal tissues may reinforce microbial dysbiosis and thus subvert the host immune response (Hajishengallis, 2015). Bacteria in the periodontal pocket may transit into the bloodstream by chewing or teeth-brushing. Hence, periodontitis may aggravate some systemic diseases (Eke et al., 2016). Furthermore, inflammatory factors such as fibrinogen and C-reactive protein (CRP) may perpetuate the destruction of periodontal tissues as well as the inflammatory response (Hajishengallis, 2017).
Peripheral artery disease (PAD) is the atherosclerotic obstruction of peripheral arteries, including the lower extremities and carotid arteries (Criqui and Aboyans, 2015; Gerhard-Herman et al., 2017). The pathogenesis of PAD is not fully understood, although both genetic and environmental factors are involved. Risk factors include hypertension, lipid metabolism disorders, smoking, obesity, diabetes, inflammation, coagulation, and disorders of the fibrinolysis system (Kullo and Rooke, 2016).
Periodontitis shares common risk factors with PAD. Both clinical and epidemiological studies suggested that there is a positive correlation between periodontal infection and increased risk of cardiovascular disease (Kullo and Rooke, 2016). Periodontal infection may be involved in the pathogenesis of atherosclerosis (Hamilton et al., 2017). The development and progression of atherosclerosis has an inflammatory component involving the production and action of various cytokines and growth factors (Geovanini and Libby, 2018). It has been suggested that local and systemic inflammation plays an essential role in the pathogenesis of atherosclerosis (Yurdagul et al., 2018; Freitas et al., 2015).
This systematic review and meta-analysis explores the association between periodontitis and PAD, and identifies potential risk factors of periodontal disease. In this way, we aim to clarify and inform future study and clinical practice.
This study was conducted according to the preferred reporting items for systematic reviews and meta-analysis (PRISMA) guidelines (Moher et al., 2009).
A systematic review and meta-analysis was conducted to evaluate the association between the incidence of periodontitis and PAD. We systematically searched bibliographic biomedical databases Ovid Medline, Embase, Cochrane Library (including Cochrane Central Register of Controlled Trials and Cochrane Database of Systematic Reviews), and Pubmed. Grey literature was also identified via Google Scholar. Keywords included: "peripheral vascular disease", "carotid", "sclerosis", and "periodontitis". Databases were searched from their inception date to 30 January 2019. All obtained studies were then imported into Endnote (Clarivate Analytic, version X6). Titles and abstracts were screened to eliminate duplicate papers.
All studies evaluating the relationship between the incidence of periodontitis and PAD were included in our study. Inclusion criteria were as follows: (i) Studies with the primary objective of identifying risk factors of periodontitis for vascular disease including LEAD and CAD; (ii) Disease was diagnosed by a qualified practitioner; (iii) Ankle brachial index (ABI) or carotid intima-media thickness (cIMT) were accurately measured to define LEAD and CAD, respectively; (iv) Both exposure to risk factors assessed by patient questionnaires, and received clinical diagnosis, were accepted as outcome measures and were included; (v) Observational studies including cohort and case-control study design were included, as well as review articles and meta-analyses. Only English articles were included.
Exclusion criteria included: (i) Animal studies; (ii) Studies wherein outcomes could not be extracted, or where no patients data were reported in both exposure and control group; (iii) Publications in the form of case reports, conference abstracts, or nonEnglish studies; (iv) Studies in which the outcome was defined other than LEAD or CAD; and (v) Studies in which the number of cases was fewer than 20.
Two investigators (JW and XG) independently screened the titles and abstracts in accordance with the inclusion and exclusion criteria. Articles that met the inclusion criteria were further examined in their entirety. In cases of disagreement, a third reviewer (HL) was consulted.
General characteristics and demographic data of each study were extracted, including author, publication year, recruitment period, country, study design, total sample, disease in question, and the sample of exposure or control group (if applicable). Outcome measures were either ABI or cIMT. Periodontitis was assessed according to the International Workshop for Classification of Periodontal Disease (Armitage, 1999), diseases such as probing depth (PD), clinical attachment loss (CAL), bleeding on probing (BOP), bleeding index (BI), plaque index (PLI) were all clarified as periodontitis. Also, the odds ratio (OR), relative risk (RR), and 95% confidence interval (CI) were calculated with primary data among studies. OR was adjusted for multivariate analysis.
Two reviewers (JS and WY) independently assessed the quality of the included papers. Since all studies were observational, the Newcastle-Ottawa Scale (NOS) was applied for bias assessment (Stang, 2010). The scale was formed with 8 question and the maximum score for each study was 9. Papers with an overall score of 7 and above was considered as of high methodological quality and an overall score of 5 and above as moderate.
All ORs and 95% CIs in each study were pooled and analyzed using Stata version 15.0 software (Stata Corporation, College station, TX, USA). The overall OR was calculated to evaluate the strength of the association between periodontitis and PAD. A P-value less than 0.05 was regarded as statistically significant. The I2 statistic was used to test heterogeneity, while the Χ2 test was used for statistical heterogeneity (I2 ≥ 50% indicating the presence of heterogeneity). If heterogeneity was identified a random-effects model would be applied, otherwise a fixed-effects model would be applied. Forest and funnel plots were drawn to assess publication bias.
Fig. 1 presents the flow chart of the screening process. A total of 3,543 studies were imported into Endnote. After removing duplicates, 1,965 were screened for title and abstract, and 86 were left for full-text screening. Sixty-one studies were excluded when reviewing full text. Ultimately, 25 studies were included based on the inclusion and exclusion criteria (Ahn et al., 2016; Aoyama et al., 2017; Beck et al., 2001; Bloemenkamp et al., 2002; Çalapkorur et al., 2017; Carallo et al., 2010; Chen et al., 2008; Desvarieux et al., 2005; Engebretson et al., 2005; Hayashida et al., 2013; Hung et al., 2003; Jung et al., 2014; Kure et al., 2018; Leivadaros et al., 2005; Lopez-Jornet et al., 2012; Mendez et al., 1998; Persson et al., 2002; Pinho et al., 2013; Ravon et al., 2003; Ramesh et al., 2013; Schillinger et al., 2006; Soder et al., 2005; Soto-Barreras et al., 2013; Wozakowska-Kaplon, 2013; Yu et al., 2014).
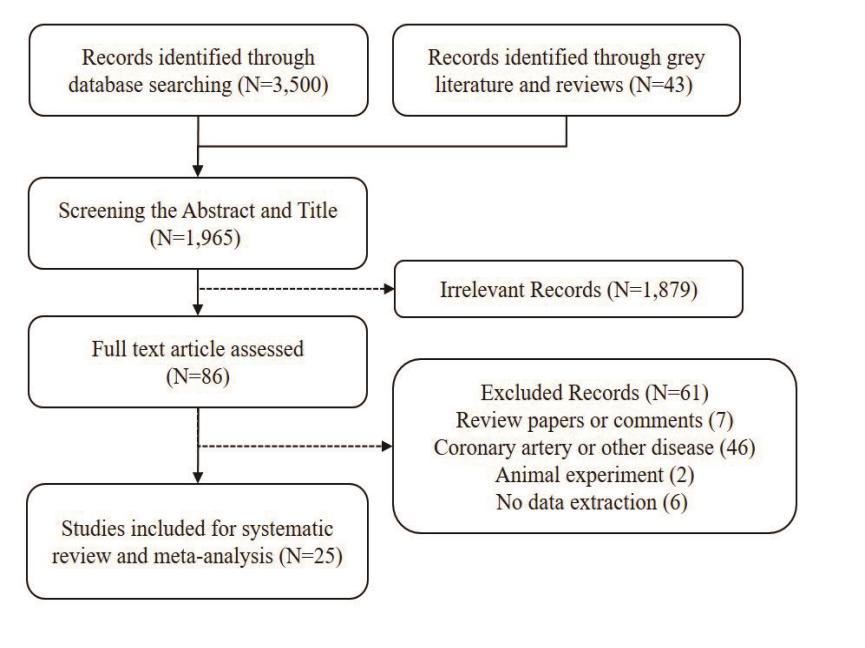 Figure 1.
Figure 1.The flowchart of the literature review. A total of 3,543 studies were systematically reviewed and 86 studies were evaluated based on the full text. Finally, 25 studies were involved based on the inclusion and exclusion criteria.
Characteristics of the included studies are listed in Table 1. A total of 22,090 subjects are included in this study. Fourteen studies were cross-sectional cohort studies, while 11 were case-control studies. Four continents (Asia, Europe, North and South America) and 14 countries (Austria, China, Germany, Italy, Japan, Mexico, Netherlands, Poland, Portugal, South Korea, Spain, Sweden, Turkey, and the USA) were covered. Seventeen studies evaluated the association of periodontitis with the incidence of, while 9 studies evaluated its association with LEAD. ABI (in LEAD patients) and cIMT (in CAD patients) were commonly used for assessing the disease. Differences existed when defining periodontitis among study articles. Quality assessment was undertaken with NOS; 16 studies received a score of more than 7 and hence were considered high quality, while the other 9 studies were of moderate quality. The adjusted or matched factors are listed in Table 2. Eight studies were not adjusted for any covariates. Fifty studies considered age, and 14 studies included smoking as covariates. Furthermore, metabolic diseases such as dyslipidemia, hypertension and diabetes, were potential confounders.
| Study (author, year) | Country | Study design | Total | Disease | Outcome assessment | Periodontitis assessment | NOS |
|---|---|---|---|---|---|---|---|
| Jung et al., 2014 | South Korea | Cross-sectional | 5359 | CAD | cIMT (B-mode ultrasonography) | number of teeth, PD, CAL, BOP | 7 |
| Yu et al., 2014 | China | Cross-sectional | 847 | CAD | cIMT ≥ 1.2 mm (M-mode ultrasonography) | PLI, PD, CAL, and BI | 7 |
| Hayashida et al., 2013 | Japan | Cross-sectional | 1053 | CAD | cIMT ≥ 1 mm and carotid plaque | PD, and CAL | 8 |
| Pinho et al., 2013 | Portugal | Cross-sectional | 50 | CAD | cIMT ≥ 1 mm (B-mode ultrasonography) | BI, PD, gingival recession, CAL | 7 |
| Ramesh et al., 2013 | USA | CADe-control | 185 | CAD | Panoramic radiographs | number of teeth, and bone loss | 6 |
| Wożakowska-Kapłon, 2013 | Poland | CADe-control | 112 | CAD | cIMT ≥ 0.9 mm (ultrasonography) | PLI, PD, CAL, BI, and number of teeth | 7 |
| López-Jornet et al., 2012 | Spain | CADe-control | 60 | CAD | cIMT ≥ 1 mm (ultrasonography) | CAL ≥ 3mm at each site | 6 |
| Carallo et al., 2010 | Italy | Cross-sectional | 33 | CAD | cIMT (echo-Doppler examination) | gingival index, BI, PD | 6 |
| Schillinger et al., 2006 | Austria | Cross-sectional | 411 | CAD | Color-coded ultrasonography | delayed missing filled teeth | 7 |
| Engebretson et al., 2005 | USA | Cross-sectional | 203 | CAD | cIMT (Doppler ultrasonography) and Carotid plaque thickness | bone loss | 6 |
| Desvarieux et al., 2005 | Germany | Cross-sectional | 1740 | CAD | cIMT ≥ 1 mm (B-mode ultrasonography) and Carotid artery plaque | bacteria identification | 6 |
| Ravon et al., 2003 | USA | CADe-control | 83 | CAD | Duplex ultrasonography | ≥ 30% of the teeth had a distance cementoenamel junction and bone level≥ 4.0mm | 6 |
| Persson et al., 2002 | USA | Cross-sectional | 1064 | CAD | panoramic radiographs | distal vertical bone defects ≥ 3mm around remaining teeth | 7 |
| Beck et al., 2001 | USA | Cross-sectional | 6017 | CAD | cIMT ≥ 1 mm (B-mode ultrasonography) | patients with ≥ 30% CAD ≥ 3 mm | 7 |
| Hung et al., 2003 | USA | Cross-sectional | 342 | CAD | angiogram or Doppler ultrasonic reports of >50% narrowing of the femoral or popliteal arteries | number of teeth | 8 |
| Leivadaros, E. et al., 2005 | Netherlands | CADe-control | 63 | CAD | cIMT (B-mode ultrasound) | radiographic cementoenamel junction and the alveolar bone crest on the teeth | 7 |
| Aoyama et al., 2017 | Japan | Cross-sectional | 988 | LEAD | Clinical symptoms, ABI, and angiographic findings | Bacteria identification, Edentulous | 6 |
| Çalapkorur et al., 2017 | Turkey | Cross-sectional | 60 | LEAD | ABI values of ≤0.90 | PD, CAL, BOP, BI | 6 |
| Ahn et al., 2016 | South Korea | CADe-control | 1343 | LEAD/ |
LEAD was evaluated by using ABI ≤1.00; |
Bone loss | 7 |
| Soto-Barreras et al., 2013 | Mexico | CADe-control | 60 | LEAD | ABI values of ≤0.90 | patients with ≥ 30% CAL ≥ 4 mm | 8 |
| Chen et al., 2008 | Japan | CADe-control | 57 | LEAD | Clinical symptoms, ABI, and angiographic findings | PD ≥ 4 mm or CAL ≥ 4 mm | 7 |
| Soder et al., 2005 | Sweden | CADe-control | 113 | CAD | cIMT ≥ 1 mm and lumen diameter (B-mode ultrasonography) | PLI, PD, CAL | 7 |
| Bloemenkamp et al., 2002 | Netherlands | CADe-control | 687 | LEAD | LEAD was angiographically confirmed when a stenotic lesion causing more than 50% reduction of the lumen was present in at least one major peripheral artery | Self-reported | 7 |
| Mendez et al., 1998 | USA | Cross-sectional | 1110 | LEAD | Defined as one of: intermittent claudication; extracranial erebrovascular disease; atherosclerosis, and arterial embolism and thrombosis. | the mean whole mouth alveolar bone loss was > 20% | 8 |
| Kure et al., 2018 | Japan | CADe-control | 50 | LEAD | CliniCAD symptoms, ABI values of ≤ 0.90 | PD, CAL, BOP | 6 |
Abbreviations: CAD = carotid atherosclerosis, LEAD = peripheral artery disease, ABI = ankle brachial pressure index, cIMT = carotid intimamedia thickness, PD = probing depth, CAL = clinical attachment loss, BOP = bleeding on probing, BI = bleeding index, PLI = plaque index
| Study (author, year) | Adjusted, or matched factors |
|---|---|
| Aoyama et al., 2017 | Age, gender, smoking, hypertension, dyslipidemia and HbA1c levels |
| Çalapkorur et al., 2017 | Age, gender, diabetes, hypertension and BMI |
| Ahn et al., 2016 | Age, gender, education level, tooth loss, smoking, drinking, central obesity |
| Jung et al., 2014 | Age, gender, year of survey, BMI, smoking, pack-years, education, medication of hypertension, medication of dyslipidemia, medication of dyslipidemia, HDL-cholesterol, log-transformed triglyceride, total cholesterol, glucose, and systolic blood pressure |
| Yu et al., 2014 | Age, gender, educational level, family income, BMI, waist-hip ratio, blood lipid level, hypertension, diabetes, and smoking |
| Hayashida et al., 2013 | Age, gender, number of present teeth, BMI, log-transformed triglycerides, HDL-cholesterol, LDL-cholesterol, HbA1c, systolic blood pressure, smoking, and habitual drinking |
| Pinho et al., 2013 | Age, gender, plaque index, bleeding on probe, dyslipidemia, and smoking |
| Soto-Barreras et al., 2013 | Age, gender, BMI, smoking, and diabetes mellitus |
| Wożakowska-Kapłon, 2013 | Age, gender, and smoking |
| Chen et al., 2008 | Age, gender, smoking, and diabetes |
| Schillinger et al., 2006 | Age, gender, BMI, arterial hypertension, smoking, hyperlipidemia, dyslipidemia, history of myocardial infarction and stroke, baseline degree of stenosis, and statin treatment |
| Soder et al., 2005 | Age, gender, BMI, heredity for atherosclerotic disease, hypertension, dyslipidemia, plasma cholesterol, smoking, and education |
| Desvarieux et al., 2004 | Age, region, smoking, DM, systolic blood pressure, high blood pressure, LDL-cholesterol, HDL-cholesterol, natural log (triglycerides), education, and BMI |
| Bloemenkamp et al., 2002 | Age, gender, smoking, and diabetes |
| Beck et al., 2001 | Race and center |
| Mendez et al., 1998 | Age, BMI, family history of heart disease, and smoking exposure |
| Hung et al., 2003 | Multi-vitamin use, Aspirin use, dentist, diabetes, hypertension, smoking |
Fig. 2 shows the overall OR and 95% CI of all included studies. Significant heterogeneity among studies was observed (I2 = 80.5%, P < 0.001). The random effects model was applied to pool ORs and corresponding 95% CIs for the meta-analysis. Among the 25 studies, only 3 studies presented a negative association between periodontal disease and PAD. Periodontitis was found to be a relevant risk factor that significantly increased the risk of developing PAD, compared to the reference group (OR: 1.60, 95% CI 1.41-1.82, P < 0.001).
 Figure 2.
Figure 2.The overall forest plot between the periodontitis and peripheral vascular disease. The overall population with periodontitis was found to be a risk, which significantly increased for developing peripheral vascular disease comparing to the reference group (OR: 1.60, 95%CI 1.41-1.82, P < 0.001).
Fig. 3 and 4 illustrate the results of the subgroup meta-analysis. Fig. 3 shows the association between periodontitis and the incidence of LEAD. No heterogeneity was observed among the nine included studies (I2 = 0%, P = 0.563). Only one study suggested a negative result. Overall, there was a significant increased risk for developing LEAD among people with periodontitis compared with the reference group (OR: 3.00, 95% CI 2.23-4.04, P < 0.001). Fig. 4 demonstrates the association between the occurrence of periodontitis and the incidence of CAD. Significant heterogeneity was observed among studies (I2 = 79.4%, P < 0.001). Yet, overall, the periodontitis cohort had a greater association with CAD than the reference group (OR: 1.39, 95% CI 1.24-1.56, P < 0.001).
 Figure 3.
Figure 3.The forest plot for detecting the risk between periodontitis and LEAD. There was a significantly increased risk for periodontitis in developing LEAD comparing to the reference group (OR: 3.00, 95%CI 2.23-4.04, P < 0.001).
 Figure 4.
Figure 4.The forest plot for detecting the risk between periodontitis and CAD. The periodontitis patients had a higher risk than the reference group in association with CAD (OR: 1.39, 95%CI 1.24-1.56, P < 0.001).
In this meta-analysis, periodontitis was related to an increased risk of PAD, not only with respect to LEAD but also to CAD. Even after covariate adjustment, periodontitis was found to be an independent variable associated with the occurrence of PAD.
Chronic periodontitis is a prevalent oral disease affecting daily life worldwide (Al-Zahrani et al., 2006). It is an inflammatory disease of periodontal tissue involving oral pathogens. PAD is another type of inflammatory disease characterized by the formation of atherosclerotic plaque (Atarbashi-Moghadam et al., 2018; Dietrich et al., 2013). Chronic periodontitis, although only overtly impacting local tissues, can lead to an increase in serum concentration of CRP, which is positively correlated with periodontitis severity (Pejcic et al., 2011). A large number of studies have demonstrated that serum CRP levels in patients with periodontitis are significantly higher than in healthy populations, even after controlling for confounding factors (Ramamoorthy et al., 2012; Ramirez et al., 2011; Zhang et al., 2016). The treatment of periodontal tissue inflammation could reduce serum CRP concentrations in patients with chronic periodontitis and invasive periodontitis. CRP concentration is also. There is evidence that CRP is a marker of both periodontitis and PAD, and that it may be a useful risk predictor for atherosclerosis in patients with chronic periodontitis (Tapashetti et al., 2014). These findings suggest the possibility of a link in the inflammatory components of both chronic periodontitis and PAD.
A large number of cross-sectional and longitudinal studies have evidenced the association between periodontitis and PAD. López et al. (2011) investigated periodontitis and atherosclerosis in periodontal patients, finding that intima-medial thickness was significantly higher in patients with periodontitis compared to those without. The percentage of CRP, white blood cell count and periodontal disease pathogen count in the periodontitis group were also observed as higher among patients with periodontitis, suggesting that untreated periodontitis is associated with early carotid atherosclerotic lesions and high levels of inflammatory markers (López et al., 2011). Chronic periodontitis has also been found to increase the incidence of PAD after controlling for confounders such as diabetes and smoking (Ahn et al., 2016), suggesting that it is an independent risk factor for PAD.
Experimental animal models have also demonstrated that periodontal disease is associated with pathogenetic mechanisms of atherosclerosis. Lalla et al. (2003) reported that apolipoprotein Edeficiency (ApoE-/-) was partially related to the prevalence of oral bacterial pathogen porphyomonas gingivalis (Pg), with concomitant increased incidence of atherosclerotic plaque. Morphological analysis in this study showed a 40% increase in atherosclerotic lesions, as well as the detection of Pg DNA in the aorta, suggesting that periodontal disease is related to the pathogenesis of atherosclerotic plaque. Mahendra et al. (2010) used 16S rRNA sequencing to study the bacterial presence within atherosclerotic plaques of 51 patients with CAD . The positive rate of Pg was calculated as 45.1%, and the positive rate of Treponema pallidum was 49.01% (Mahendra et al., 2010). In INVEST, 4,561 samples of subgingival plaque were analyzed through 657 dental examinations (Bernal-Pacheco and Román, 2007). Eleven kinds of bacteria were detected by DNA-DNA hybridization, and the number of periodontal bacteria present was associated with cIMT (Bernal-Pacheco and Román, 2007). These studies provide evidence that periodontal pathogens can be detected in the CAD, as well as suggesting that they influence the formation of atherosclerotic plaque, possibly reaching arterial lesions through the vascular circulation (Bernal-Pacheco and Román, 2007). Li et al. (2002) also found that the long-term effects of Pg accelerate the formation of atherosclerotic plaques in a ApoE(-/+) heterozygous mouse model. In this study, intravenous injection of active Pg in mice led to earlier and more pronounced plaque formation in the aortic arch (Li et al., 2002).
Periodontitis and PAD share common risk factors such as smoking and diabetes. A mechanism by which periodontal disease influences the pathogenesis of PAD is proposed as follows. Firstly, periodontal pathogens or their components directly enter the bloodstream. This may occur, for example, by tooth extraction and subsequent bacteremia, whereby blood-borne bacteria may directly invade the vascular endothelial and smooth muscle cells (Amar et al., 2003). Hence, secondly, a systemic inflammatory response is induced. The more severe the periodontal disease, the more significant the systemic inflammatory response causes an increase in the concentration of inflammatory cytokines in the blood (Ahmed et al., 2014). The similarity between bacterial and host peptides (known as molecular mimicry) may induce an autoimmune response and, in the presence of predisposing factors, may accelerate atherosclerotic plaque formation (Alfakry et al., 2011). Further, periodontal pathogens may promote the oxidation and aggregation of low-density lipoprotein, which are then internalized by microphage phagocytosis, thus forming foam cells, which are the primary component of the fatty streak or early-stage atherosclerotic lesion (Goteiner et al., 2008; Champaiboon et al., 2014).
This meta-analysis comprehensively explored the risk of periodontitis for PAD. While we identified heterogeneity among the included studies (as shown in both the overall and CAD forest plots), this may be related to inconsistencies in the definition of CAS and periodontitis, as well as their methods of assessment. It is possible, too, that undefined covariates, such as dietary habits, had an impact upon outcomes observed; although certain measured covariates were adjusted for, the possibility of bias remains.
There were some limitations to this study. Firstly, although a total of 22,090 participants were identified among included studies, data on individual patients was unavailable. Secondly, no randomized controlled studies were identified. Furthermore, the restriction to the English language alone, and narrowed geographical coverage, may be potential sources of bias.
Our meta-analysis of 25 studies identified by comprehensive systematic review indicates that periodontitis is an independent risk factor for the increased incidence of both CAD and LEAD.
The author wanted to appreciate the funding from Heibei Science and Technology Project (13277184).
The authors declare no conflicts of interest statement.
