Since the discovery of the first microRNA (miR), almost three decades ago, the roles played by miRs under normal and diseased settings have been widely investigated. miRs are found to play crucial roles in cancer initiation and progression, as well as towards therapy response mechanisms. Therefore, they are relevant and attractive targets for therapeutic development. Many preclinical studies have demonstrated their promise as future anti-cancer tools. Recently, increasing number of early phase clinical trials have emerged. In this Commentary, we will summarize the major discoveries within the miR research field and highlight the status quo of current miR-therapeutics, which has prominent potential of impacting future cancer regimens given their massive dysregulation in oncogenic processes.
In 2021 Frontiers in Bioscience-Landmark has reached its 25th anniversary, and this Commentary presents an opportunity to acknowledge the success of one of its most highly-cited papers, i.e., the 2019 article by Dai et al. [1], which focuses on the role of microRNA (miR)-21 in Non-Small Cell Lung Cancer (NSCLC). miR-21 will serve as Ariadne’s thread in this mini-review, in which, miR-21 is adopted as a narrative guide to summarize the major discoveries obtained in the microRNA field, a term coined back in 2001 to classify this distinctive class of small untranslated RNAs [2, 3, 4, 5, 6, 7].
Since 1993, when the 22 nucleotide-long RNA lin-4 was first identified [8], thousands of other microRNAs have been discovered to possess post-transcriptional gene regulation properties in RNA-based gene silencing processes in eukaryotes. lin-4 is rightfully considered as the founding member of miR biomolecules, and its discovery has shifted the paradigm on gene regulation, which has been based on the “central dogma” of genetics where DNA is first transcribed into messenger RNA (mRNA), and then translated into protein.
Within the genome, miRs are often found as clusters from which they are
transcribed as discrete polycistronic transcripts, or share the promoter of host
genes and are spliced from their mRNA transcripts during biogenesis [9]. miR-21
was one of the first mammalian microRNAs identified [3] and the first to be
elucidated on the mechanism of miRs processing starting from pri-microRNAs
(pri-miRs) [10]. These ~1-kb-long transcripts form a
characteristic hairpin structure that undergoes nuclear processing through
cleavage by the Drosha/DGCR8 ribonuclease complex [11, 12]. Afterwards, they are
released into the cytoplasm as ~60 nucleotides-long precursor
hairpins called pre-miRs, via an Exportin 5 and Ran-GTP complex. Subsequently,
their ends are cleaved by the Dicer/TRBP complex resulting in the mature
double-stranded miR duplex [13]. At this stage, only one strand of the miR
duplex, the guide strand, is loaded onto Argonaute (Ago) to form the RNA-induced
silencing complex RISC [14, 15]. This dynamic process eventually results in the
production of mature miR that physically interacts with a complementary or
partially complementary sequence usually located in the 3
Given that a single miR can regulate a variety of target genes, and that a
single protein-coding gene usually contains several miR seed sequences, the miR
regulatory system stands en bloc as a complex mechanism regulating
eukaryotic gene expression. It is estimated that miRs may regulate
Cancer is defined by abnormal cell division and differentiation, and can arise not only from alteration of various molecular mechanisms including dysregulation of several protein coding genes but also global changes in miR profiles. Despite miRs being the most widely studied class of non-coding RNAs, other components of the non-coding machinery such as the recently-discovered RNA species small nucleolar RNAs (snoRNAs), small interfering RNAs (siRNAs), transcription initiation RNAs (tiRNAs), PIWI-interacting RNAs (piRNAs), transcribed ultra-conserved regions (t-UCRs) and large intergenic noncoding RNAs (lincRNAs) [30, 31, 32] will certainly be identified as significant players in our war against cancer, once we can adequately delineate their complex biology.
The first evidence showing that miRs were dysregulated in human cancer came from
studies on B-cell chronic lymphocytic leukemia (CLL), in which a critical region
on chromosome 13q14 has been found to be frequently deleted in CLL, and that that
this deleted region contained two microRNA genes (miR-15a and miR16-1) [33].
Subsequently, microRNA genes were identified at fragile sites and genomic regions
involved in chromosomal alterations identified in various human tumors [34], and
defects in miR-mediated regulation can noticeably lead to human cancers [35].
Several other mechanisms controlling altered miR expression in cancer have been
reported comprising mutations [36], small nucleotide polymorphisms (SNPs) as
described in lung cancer [37], DNA methylation (consistently half of the genomic
sequences of miR genes are associated with CpG islands) [38], DNA hypomethylation
leading to miR upregulation [39, 40] and histone acetylation [41, 42]. Not
surprisingly, another dysregulated regulatory mechanism entails that some
oncogenic mRNAs carry mutations or SNPs in their 3
Large-scale profiling of gene expression in multiple human cancers have shown that one of the most frequently dysregulated gene in cancer is miR-21, frequently found overexpressed in all tumor types including lung cancer [48, 49, 50]. miR-21 expression within the tumor microenvironment (TME) is currently under-investigated when compared to tumor cells per se. However, we are beginning to comprehend its key relevance in the TME, which is to be considered as the most tumor-intermingled “organ” and symbiotic with cancer cells. In tumor-infiltrating macrophages, miR-21 inhibition for example, is pivotal in regulating tumor progression [51]. In addition, miR-21 (and miR-29a) which is secreted by tumor cells in exosomes, better defined as small extracellular vesicles (sEVs) [52, 53], can interact with members of the TLR (Toll-like receptors) family to stimulate TLR-mediated pro-metastatic inflammatory response on tumor associated macrophages (TAMs), thus suggesting a new mechanism of miR-TLR mediated intercellular communication between the TME and cancer cells [54]. Interestingly, sEVs produced within the TME by cancer-associated adipocytes (CAAs), TAMs, and cancer-associated fibroblasts (CAFs) contain miR-21, and sEVs-mediated miR-21 delivery into cancer cells is shown to confer therapeutic resistance in multiple cancers [55, 56], suggesting apart from cancer cells, the TME should also be targeted with anti-miR-21 therapeutics.
A role for miR-21 as an oncogenic miR (oncomiR) was demonstrated in vivo using a doxycycline-inducible miR-21-LoxSTOPLox-Tet-off mouse model [57], that upon induction, displayed malignant pre-B cell lymphoid-like phenotype. A parallel study demonstrated a pro-tumorigenic role of miR-21 in NSCLC where deletion of miR-21 in a KRAS-driven lung cancer model reduced tumorigenesis, while mir-21 overexpression showed the opposite effect [58]. Additionally, amplification of chromosomal 17q23.2 region, which includes miR-21, has been observed in breast, lung, hepatocellular, ovarian and prostate cancers [59]. Further, TCGA data demonstrate the locus containing miR-21 is amplified, and that such amplification can act as a prognostic marker in pulmonary adenocarcinomas [60]. miR-21 expression can also be upregulated via transcription factors that are upregulated in cancer such as AP-1 that acts down-stream of RAS and binds to miR-21 promoter [61, 62]. Other factors implicated in miR-21 upregulation are STAT3 [63] whose high expression is associated with poor patient outcomes [64, 65, 66] and NF-kB [67]. However, the complexity of the predicted promoter region of pri-miR-21 [61, 68] and occurrence of alternative transcription start sites [69] suggest that regulation of miR-21 transcription may not be a straight forward process [70]. Not surprisingly, miR-21 is upregulated by one of the most lethal oncogenes, i.e., BMI-1. BMI-1 is responsible for maintaining the self-renewal ability of cancer stem cells in virtually all tumors, including lung cancer [71, 72, 73]. In gastric cancer, BMI1 can upregulate miR-34a, which appears to have opposite effects than miR-21, hinting the presence of a negative feedback loop between BMI1 and miR-34a, through which BMI1 can regulate its own function [71]. The interplay between BMI1 and miR-21 in lung cancer is still undefined; however, BMI1 may form regulatory networks with other relevant miRs. For example, we identified miR-192 as one of the main upregulated miRs upon treating lung cancer cells with PTC-209, a compound capable of inhibiting BMI1 activity. This prevents cell cycle progression by arresting cells in G0. miR-34a was upregulated, although at a lower extent than miR-192, whereas, miR-21 levels remained unaffected (Maroni and Levantini, personal communication) thus implying that different miRs, other than miR-21, may constitute the BMI1 oncogenic regulatory network under different conditions.
Given miRs are highly dysregulated in cancer, the potential for miR signatures to distinguish not only between tumor and normal tissue, but also to identify different subgroups of tumors and predict outcome or response to therapy treatments has been intensely investigated. Our ability to adopt them as biomarkers, however, is still in the infancy stage. Inconsistent results were frequently reported by different research groups and these may arise from differences in stage and treatment received by patients of the analyzed samples. Therefore, large scale studies are needed and preferably should be carried out at multicenter locations to ensure higher patient recruitment, with strict screening criteria and higher statistical power when assessing sensitivity, specificity and pertinence of miRs as future biomarkers. However, successful observations have been reproduced and one evidence that has been stratifying over the years, is the role that miR-21 plays in restricting response to therapy and causing drug resistance by regulating expression of resistance-related factors in multiple cancer types. One of the first reports describing miR-21 involvement in chemo-resistance was shown in cholangiocarcinoma cells, in which its (and miR-200b’s) inhibition led to increased sensitivity to gemcitabine [74]. miR-21 overexpression is related to development of Multi Drug Resistance in breast cancer [75], in which its downregulation improves the chemotherapeutic effect of Taxol [76]. miR-21 inhibition is shown to be directly responsible for PTEN expression and re-sensitivity to doxorubicin via increased caspase-related apoptosis [77]; and its inhibition, associated with co-delivery of the cytostatic compound docetaxel within “chitosomes”, improves chemo-sensitivity to the compound [78]. Near-infrared-radiation-responsive hollow gold nanoparticles have been adopted to achieve sequential delivery of miR-21 inhibitor and doxorubicin, in breast cancer xenograft models. They displayed successful tumor delivery followed by effective accumulation, that resulted in good therapeutic efficacy, showing the potentiality of the “sequential delivery concept” for cancer therapeutics settings [79]. Similarly, simultaneous systemic administration in exosome nanocarriers of the cytostatic drug 5-FU and a miR-21 inhibitor oligonucleotide demonstrated major anti-tumor effects in a colon cancer mouse model [80]. In gastric cancer, the same combination of 5-FU and miR-21 inhibitor was delivered in trastuzumab-conjugated nanoparticles, which increased trastuzumab targeting and antibody-dependent cellular cytotoxicity while enhancing sensitivity of gastric cancer cells to trastuzumab and 5-FU [81]. There is growing evidence that delivery of miR therapeutics together with chemotherapeutics can improve treatment efficiency, and miR-21 is one of the most extensively studied miR therapeutics in combination-delivery settings, given its protagonist role in various tumorigenic settings [78, 79, 80, 81].
Higher expression of miR-21 has been reported in plasma [82] and tissues [83] from NSCLC patients, as compared to healthy donors. Additionally, it has been identified as a useful predictor for early detection and chemo-sensitivity biomarker in plasma from patients with advanced NSCLC [84, 85]. Further, miR-21 has been implicated in the development of gefitinib resistance in EGFR mutant NSCLCs [86]; as well as resistance to cisplatin, gemcitabine, 5-fluorouracil and teniposide in various cancers [75, 87, 88, 89, 90, 91, 92, 93, 94, 95]. It has alone been correlated with the development of brain metastases in NSCLC patients [96] and its inhibition could improve sensitivity to radiotherapy in the NSCLC cell line A549, mediated by the PI3K/Akt pathway [97]. Consistently, miR-21is a part of a defined signature (containing seven miRs) capable of predicting response to platinum-based treatments [98]. As biomarker, miR-21, belongs to a novel panel of serum-based miRs capable of discriminating breast cancer patients and healthy controls [99]. miR-21 possesses the highest specificity and sensitivity in NSCLC patients’ sputum or plasma [84, 100]; and it is a common component to several molecular signatures for NSCLC diagnosis [101, 102, 103] where high plasma sEV miR-21 levels are shown to associate with poor overall survival (OS) [104]. On the basis of the above considerations, miR-21 can serve as an attractive candidate as a potentially relevant biomarker for diagnosis, prediction, and prognosis [105, 106, 107, 108] though, it has not been adopted in the clinic presently [109]. However, it should also be taken into account that not all that glitters is gold, and that miR-21’s utility as a biomarker may be a double-edged sword. miR-21 ubiquitous overexpression in virtually all cancers represents the biggest challenge which is specificity. miR-21 may not be the most suitable biomarker for a specific type of cancer but rather a broad “alarm-miR” which is indicative on the presence of oncogenesis and may require coupling with more tissue/organ-specific biomarkers. The evidence presented suggest a great possibility that miR-21 to be adopted in the screening for lung cancer, which is the deadliest malignancy worldwide.
NSCLC, that we investigate in my laboratory, accounts for more than 80% of all lung cancer cases [110]. It is essentially untreatable, although many strategies have been proposed to improve patients’ survival. Most patients are diagnosed at an advanced stage and half of cases have distant metastatic disease at initial diagnosis, with poor prognosis. As a result, there is a major need to identify faster and non-invasive ways to detect lung cancer at early stages. miRs, as biomarkers, may fulfil this request after we have successfully understood how to employ them in the correct manner. Aberrant miR signatures are commonly observed in NSCLC and they are most frequently associated to upregulation rather than downregulation [111, 112, 113, 114, 115, 116, 117, 118, 119, 120, 121, 123]. These abnormally overexpressed miRs represent a valuable repertoire from which the proper panel of biomarkers can be selected for association to “alarm-miR-21” in the design of non-invasive tests for next-generation NSCLC detection.
Certainly, additional basic research is required before miR-21 can be
extensively adopted as an approved biomarker. However, its upregulation in
numerous types of cancer and association with cancer-related pathways renders it
a promising molecule for RNA-based therapies. miR-21 regulates various downstream
effectors associated with tumor pathogenesis during all stages of carcinogenesis
as it is involved in regulating signaling pathways implicated in apoptosis, cell
growth, proliferation, survival, angiogenesis, migration, extravasation, invasion
and metastasis, and also chemo- and radio-resistance pathways [57, 58, 124, 125, 126, 127, 128, 129, 130, 131, 132, 133, 134, 135, 136, 137, 138, 139, 140, 141, 142, 143, 144].
Dai et al. [1] corroborated the existence of an inverse relation between
miR-21 and PTEN in NSCLC, that is also observed in other cancers [143, 145, 146, 147, 148, 149, 150].
Specifically, they demonstrated that miR-21 regulates lung cancer proliferation,
cell cycle progression and EMT, through the PTEN/Akt/GSK3
Several experiments aimed at affecting miR-21 have been performed over the years. When a miR-21 antagomir was used in breast cancer cells, tumor growth was restricted through inhibiting cell proliferation and inducing apoptosis [151]. Additionally, synthetic circular RNAs (circRNAs) that could function as miR-21 sponges, thus acting as competitive inhibitors, have been developed to inhibit miR-21 activity which displayed inhibition of cell proliferation in gastric cancer [152]. Intra-venous administration of MKAD-21 (a chemically modified antisense oligo against miR-21) in xenograft models could dose-dependently suppressed bladder cancer growth through regulation of the PPP2R2A-ERK network, which is a mediator of miR-21-induced oncogenesis in bladder cancer [153]. Anti-miR-21(AM-21), composed of two cationic lipids, has been therapeutically used in a preclinical murine model of lung cancer, in which it displayed reduced tumor growth with prolonged survival without toxicity [154].
As a naturally occurring class of gene regulators, microRNAs have attracted great attention as promising targets for therapeutic development, given their knack for targeting virtually any gene of interest at the post-transcriptional level. Tumor progression is caused by the deregulation of multiple cellular pathways, therefore the combinatorial ability miRs display to target multiple disease-related genes concurrently, may provide an advantage, as compared to traditional small molecule therapeutics. Both viral and non-viral carriers, have been utilized to develop miR-based therapies aimed at either reducing the expression of specific oncomiRs (by means of antimiRs/antagomiRs based on antisense oligonucleotides (ASO), locked nucleic acid (LNA) antimiRs, or tiny LNA antimiRs) or at replenishing rare tumor suppressing-miRs (by means of synthetic and/or chemically-modified miR mimics). Nowadays, the miR therapy road is still paved with several challenges (Fig. 1) that need to be addressed (mainly identification of potential off target effects and improved delivery methods) before their effective translation into future therapeutic applications can take place.
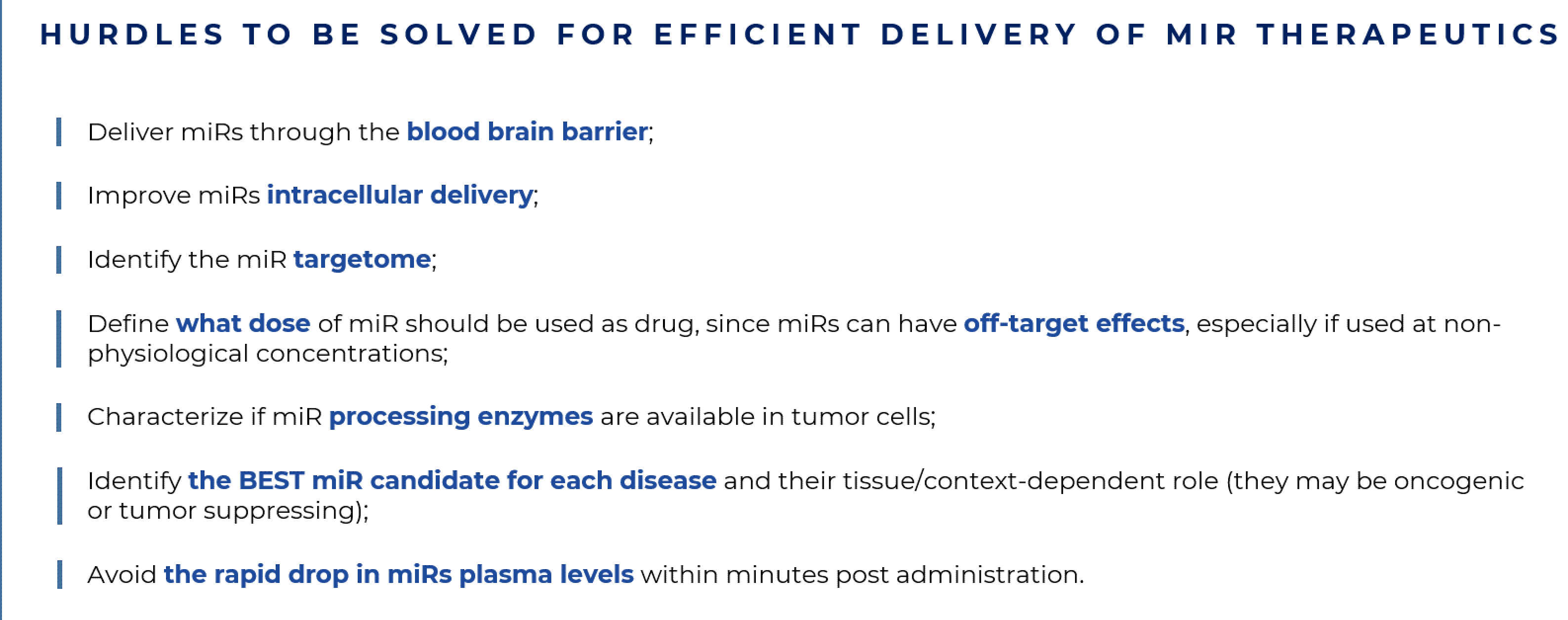 Fig. 1.
Fig. 1.Hurdles to be solved for efficient delivery of miR therapeutics.
In primis, in order to truly enter the era of RNA therapeutics, it is necessary to identify the best miR candidates or miR targets for each disease, as well as understand if a specific miR (and its targets) follows a unidirectional function/behavior of oncomiR or tumor suppressor, or if their role changes in different tissues/conditions. This information is relevant to decide whether miR inhibitory or miR mimics therapeutic strategies can be utilized in each specific disease-driven scenario. At the present stage, we should also consider an extra level of complexity; i.e., the major heterogeneity displayed by tumors and their intermixed TMEs, which can be patient-specific and represents a major obstacle in identifying the relevant target miRs to adopt each time. Despite tumor cellular heterogeneity, functional heterogeneity governed by factors such as hypoxia and inflammation can cause dynamic localized heterogeneities [28, 155, 156, 157, 158, 159]. miR biogenesis enzymes such as Drosha, Dicer and AGO2 are downregulated by hypoxia, further destabilizing miR expression [157, 158, 160, 161] and complicating the identification of candidate miRs.
Currently, the molecular characterization of tumors is predominantly derived from analyses of bulk tissues, and the application of single cell RNA sequencing (scRNAseq) techniques should bring major advances in our understanding of how transcripts (both non-coding and coding) perform at the single-cell molecular level, and how they are affected in contexts as various as tumor initiation, response to drug treatment, and development of therapy resistance. Given miRs’ mechanisms of action, the amount of miR within a cell can dictate the impact on gene expression. Therefore, quantifying single cell miRs levels will be great interest to study their expression in defined subpopulations (identified by scRNAseq as distinct transcriptional clusters) contained within tumors and TMEs. As mentioned above, miRs can essentially exert dual roles and function as both oncogenic or tumor suppressive units. However, they can even act in a context-dependent manner and exert different roles in suppressing or enhancing tumor progression. miR-141, for example, was reported to be a tumor-suppressive miR by counteracting Tregs recruitment and immune escape in advanced-stage NSCLC patients with malignant pleural effusion [162]. However, the same miR is shown to be oncogenic by targeting tumor suppressor genes PHLPP1 and PHLPP2 in NSCLC and inducing the proliferation of cancer cells [163]. Similarly, members of the miR-29 family, comprising three isoforms (miR-29a, miR-29b and miR-29c) can act as tumor-suppressors in mantle-cell lymphoma, acute myeloid leukemia (AML), lung cancer, diffuse large B cell lymphoma and Burkitt lymphoma, and oncogenic miRs in indolent human B cell chronic lymphocytic leukemia, AML and metastatic breast cancer [164, 165]. The miR143/145 cluster is a tumor suppressor in cancer cells however, it can also induce neo-angiogenesis in the TME leading to increased tumor growth [166]. To achieve a better response to treatments, through miR-based cancer therapy, it is anticipated that miRs are required to be downregulated or upregulated in a tissue- or context-dependent manner. Regrettably, this level of accuracy is not achievable at this present stage.
Further, miRs affect multiple target genes hence it is difficult to predict and evaluate all their potential off-target effects [167]. For example, when a target gene has functions that can either promote or suppress the carcinogenic process [168] such as the miR-21 target BCL2 [169], the effectiveness of a miR-based therapeutic option is questioned. Also, the ability of miRs to target several genes involved in disease is a bonus as it helps with the targeting of the entire lineage of disease-related genes, but this intrinsic feature may also favor the introduction of off-target effects [170]. Thus, elucidating the entire and extensive network of interactions displayed by miR-target genes (the miR targetome) is the gold standard to take miRs one step further towards therapeutic application. Only when such knowledge is available, well-designed therapeutic methods can be implemented to unambiguously slow down tumor growth, and preventing drug resistance and metastases, even in personalized medicine protocols.
An additional hurdle to consider is the ability to design appropriate parenteral delivery systems capable of specifically and effectively target cell types/tissues/organs and to ensure high stability, efficient uptakes by the cells and proper localization of the miR sequence into the cytoplasm [171, 172, 173]. Another concern is the use of miR drugs at non-physiological concentrations as they may exhibit a different targeting scenario than usual and can dysregulate gene expression in unanticipated manners. An even more critical factor required for the activity of miR drug processing is the amount of physiological RISC complex available, given that RISC proteins are abnormally downregulated during hypoxia [174], which is frequently associated to tumorigenesis hence creating a catch-22 situation. Sufficient expression of RISC complex proteins should be first evaluated while treating with exogenous miRs, considering that limited RISC expression may create competition between exogenous and endogenous miRs [175] thus diminishing the effectiveness of treatment overall. Finally, the complex extracellular matrix surrounding solid tumors may impede the delivery of any compound to cancer cells, and non-malignant cells may concomitantly sequester miR drugs from the tumor area. All these parameters can significantly contribute to a reduced presence of miR therapeutics in the TME, and consequently lead to inefficient uptakes into tumor cells. The ability to directly target dysregulated miRs in tumor cells or in tumor-infiltrating cells and/or cancer-associated fibroblasts or endothelial cells would have significantly improved treatment regimens however, such delivery technique is a chimera that we are still chasing. Overall, some progress has been made, but we still have a lengthy journey ahead before miR therapies are fully optimized for cancer treatment [176, 177].
miRs are water-soluble which endow properties that are appropriate for parenteral administration. Unfortunately, following i.v. injection, naked miRs are rapidly degraded by the abundant nucleases present in the extracellular and plasma environment [178] and removed from the circulation [175], thus causing a rapid drop in plasma levels within minutes post administration. Delivering miRs via systemic administration by using antibodies, ligands, and nanoparticles, or even by directly injecting the drug at pathogenic site, can enhance target specificity and efficacy, as well as minimize side effects [175, 179]. However, the latter is impractical for treating metastasizing tumors and leukemias [180]. Another challenge is the ability of delivering miRs through the blood brain barrier (BBB). Partial success has been obtained by adopting intranasal administration and modified micelle, liposomes, or nanoparticles, given only lipid-soluble small molecules are able to cross the BBB [181, 182]. Recent findings have revealed that miRs can be drugged with small molecules, i.e., small-molecule inhibitors of miRs (SMIRs) and small-molecule degraders (SMDs) that target miRs directly. The first SMIR was developed against miR-21 [183]. SMIRs bind to miRs and inhibit their biogenesis and maturation, while SMDs bind to miRs and induce their degradation [184, 185]. These small molecules will pave the way for the development of novel therapeutics against miRs that only recently were considered druggable.
Presently, despite some phase I/II clinical trials, the era of phase III compounds is still a moving target. A prominent example of a miR drug that encountered problems in clinical trials is MRX34, a mimic of naturally occurring miR-34, that was terminated at the phase I study due to serious immune-related adverse events and later on, a planned phase II study in melanoma patients was withdrawn [186]. A more favorable outcome occurred to the first TargomiR (miR-15/16 mimics packaged in nano-cells targeted with EGFR antibodies) that was tested in a phase I study on patients with malignant pleural mesothelioma [187], showing an acceptable safety profile thus supporting additional studies of TargomiRs in combination with chemotherapy or immune checkpoint inhibitors [188]. Similarly, Cobomarsen (MRG-106), a locked nuclear acid-based anti-miR, which targets miR-155 in multiple hematological malignancies, is shown to be safe in a phase I study.
This small excursus on miR-based medicine shows that the possibility to adopt them as pharmaceuticals is still in its early stages and that several strategies have been designed to efficiently deliver them (Fig. 2).
 Fig. 2.
Fig. 2.Strategies to treat patients with miR therapeutics. Both single molecule (left panel) and combination strategies (right panel) are tested in pre-clinical settings to design efficient and proper delivery in patients of miRs or miRs combined to chemotherapeutics.
There is considerable interest in using miR drugs in pulmonary diseases. Direct intrapulmonary administration, with or without aerosolization, has been adopted in murine models of pulmonary hypertension [189, 190, 191, 192, 193]. A meritorious paper from Schlosser et al. [194], systematically investigated the relative pros of intratracheal and intranasal routes of administration, with and without aerosolization, and comparing them with intravenous, intraperitoneal and subcutaneous injection. Pulmonary levels of the miR mimic showed variations by up to 4 orders of magnitude between different delivery methods thus demonstrating the impact of both the route of administration and mimic formulation. Although all methods showed elevated lung levels, intratracheal and intranasal routes of administration were clearly superior for lung-selective targeting. This selectivity was evidenced by pulmonary levels that were at least 10-fold, and up to 10,000-fold, higher than levels observed in other tissues. In applications where lung-targeted mimic delivery is not an essential requirement, intraperitoneal and subcutaneous administration could serve as alternative methods to increase lung miR levels without the need for anesthesia [194]. Previous studies have indicated that some aerosolized materials may be distributed more uniformly within the lungs [195, 196]; and in a proof-of-concept study, the delivery of miR-17 to bronchial epithelial cells (BECs) using nebulized lipid-polymer hybrid nanoparticles (LPNs) showed efficient and well-tolerated delivery of miR mimics to BECs [197].
In lung cancer, miR-21 has been considered as a potential gold standard for personalized therapy given its heavily-documented oncogenic role. Advancements in RNA chemistry and delivery technologies are encouraging for a potential future use of miR-21 as part of the standard treatment for NSCLC [198]. Recently, a nano-cellular (minicell) delivery vehicle loaded with miR-16-5p mimics was designed to target tumors via minicell-surface attached bispecific EGFR-targeting antibodies (EnGeneIC Dream Vectors - EDVs), upon intravenous injection [199]. Preliminary data presented by Van Zandwijk et al. [188] from phase I clinical trials for patients with Malignant Pleural Mesothelioma and advanced NSCLC showed manageable safety profiles in 5 patients [199].
Early phase clinical trials, aimed at suppressing miR-21, are currently ongoing. RG-012, a chemically-modified oligonucleotide capable of binding miR-21, is currently being tested in phase I on patients affected by Alport syndrome, and initial data showed that the rate of progression of renal fibrosis is reduced (ClinicalTrials.gov: NCT03373786). In addition, an interventional clinical trial is currently being conducted that involves the study of six miRs (including miR-21) to determine whether a patient with stage II colon cancer is a candidate to receive adjuvant chemotherapy based on OS and disease-free survival (DFS) measurements (ClinicalTrials.gov: NCT02466113).
Overall, experimental and clinical evidence demonstrate that miR-21 is a promising biomarker (for diagnosis, prognosis and prediction) in tumorigenesis, as it is commonly dysregulated in virtually all types of cancer. Identification of its target genes and the effects of their downregulation remains to be fully elucidated. In vitro and in vivo studies have shown that its inhibition has anti-tumor effects, thus advocating for its promising therapeutic function [200]. Presently, clinical trials and toxicity pharmacokinetic evaluations are being conducted for miR-21 inhibitors however several limitations for its use still exists such as the lack of knowledge on dose requirements as well as delivery strategies and identification of side effects. Work on these limitations is currently underway and current techniques are being designed to mitigate such issues, and to maximize therapeutic efficacy. The overall progress in developing miR therapeutics within the short time frame, since their discovery, is noteworthy [201]. Nevertheless, several well-designed preclinical studies, coupled to novel delivery platforms, are strictly required to explore the promising potential of RNA therapy. These findings will serve as catalysts for the new era of RNA-based therapeutics, especially for miRs, that are markedly dysregulated in cancers.
Not applicable.
EL acknowledges Azhar Ali, Igea D’Agnano, Giorgia Maroni, for helpful discussion and Elisabetta Pisano (Communication Office, Institute of Clinical Physiology, CNR, Pisa, Italy) for graphical design.
This work is funded by MIUR (Ministry of Education, University and Research) Flagship Interomics Project 20/2017 to EL, and sponsored research support from PTC Therapeutics to EL.
The author declares no conflict of interest. EL is serving as one of the Editorial Board members of this journal. We declare that EL had no involvement in the peer review of this article and has no access to information regarding its peer review. Full responsibility for the editorial process for this article was delegated to GP.
