Academic Editor: Tao Wang
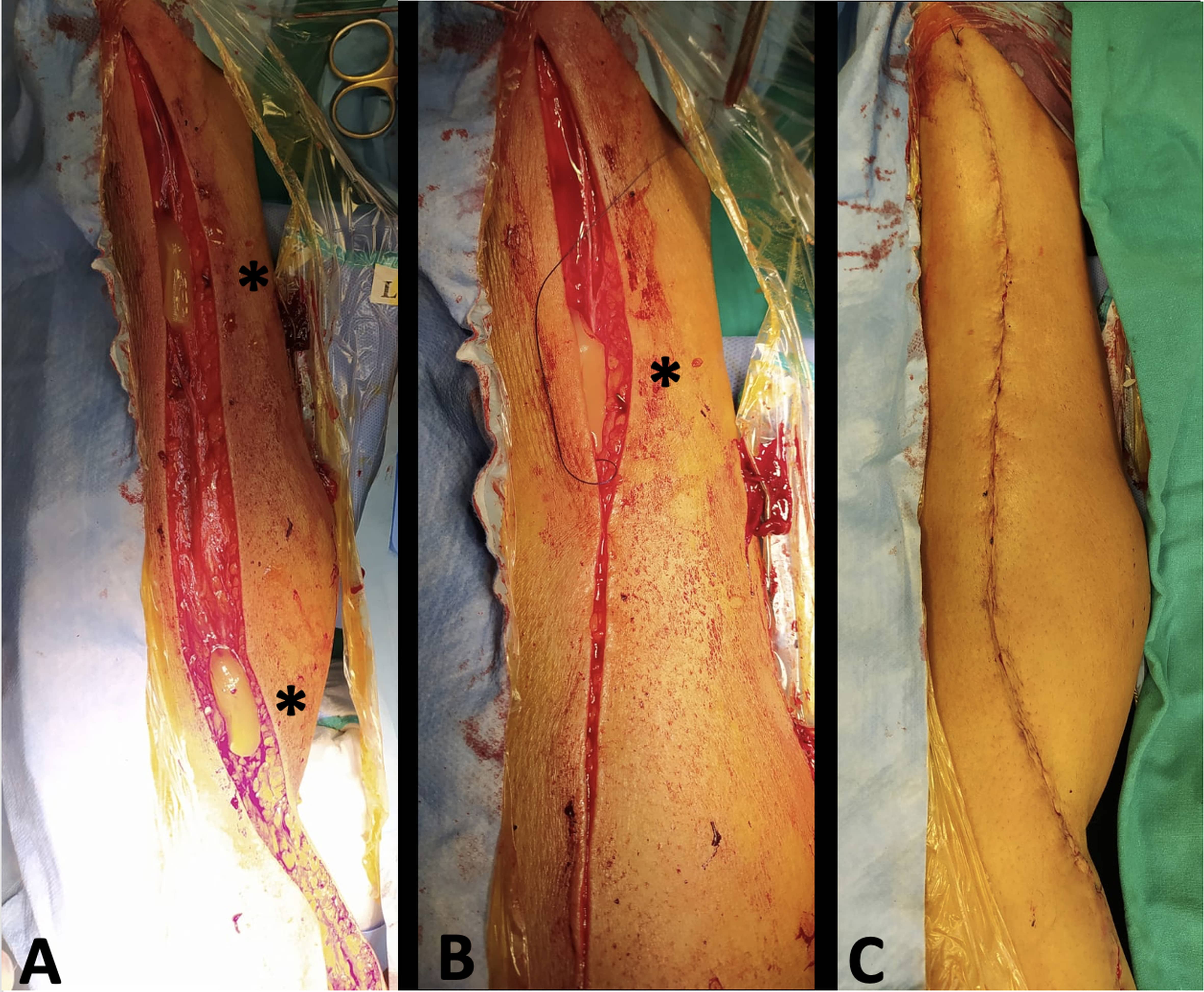
Background: Wound infection represents a frequent trouble following
open saphenous vein harvesting in cardiac surgery. Platelets’ growth factors are
crucial for the healing process. Prophylactic platelet rich plasma (PRP)
application on leg wound might reduce the incidence of saphenous vein harvest
site infections in patients undergoing coronary artery bypass graft surgery
(CABG). Methods: Between January 2009 and December 2020, 987 consecutive
patients underwent CABG using saphenous vein as conduit graft and were
retrospectively divided into two groups. All patients had standard surgical leg
wound closure and wound care, but treatment group received adjunctive topical
application of PRP (no-PRP and PRP group, respectively). The primary outcome was
wound infection. Results: Saphenous vein harvest site infection
rate was similar between PRP (3.5%) and No-PRP (5.2%) group, p = 0.215. The
ASEPSIS score was lower for the PRP group (PRP: 3.6