3D printing is a rapidly advancing technology which represents a significant technological achievement that could be useful in a variety of biomedical applications. In the field of surgery, 3D printing is envisioned as a significant step in the areas of surgical planning, education and training. The 3D printed models are considered as high quality and efficient educational tools. In this paper A randomized controlled trial was performed to compare the educational role of 3D printed models with that of the conventional MRI films in the training of surgical residents. Statistical analysis revealed that Resident surgeons who studied only the anal fistula printed models, (Group B) achieved a higher overall score in the fistula assessment test (87,2 (82,6-91,6)) compared to resident surgeons (Group A) who studied only MRI images (74,85 (66,8-73,5)). 3D printing technology can lead to improvement in preoperative planning accuracy, followed by efficient optimization of the treatment strategy. It is believed that 3D printing technology could be used in the case of various other surgical applications, thus representing a novel tool for surgical education.
Three-dimensional (3D) printing is a well-established, rapid prototyping, additive manufacturing technology. This technology offers a revolutionary opportunity of creating parts and components in bulk from different materials exhibiting the desired mechanical and physical properties. As a result, 3D printing has been considered as a significant technological innovation in medicine with a wide variety of applications to overcome existing limitations, while at the same time providing significant improvements to the state-of-the art technologies. Clearly, it could be used to create 3D anatomical models for better preoperative planning (1), optimization strategies for device testing (2) and surgical educational proposes (3). Moreover, the generation of a prototype 3D model based on patient-specific analytical image findings offers micro-scale anatomical precision and reproduction in a time-efficient manner. Till now, the most important application of 3D printing in the medical field has been the design and development of medical devices and instrumentation (4, 5). Recently, 3D printing has received significant attention from surgeons that have been able to plan complex operations in a better and more efficient manner with the use of 3D-printed anatomical models (6-8). These models could be useful for educational purposes and appear to be easier to handle, as well as it is more cost-effective as compared to cadaveric models.
Anal fistulas originate from the anal glands at the dentate line and lead to abnormal communications between the anal canal and perianal skin. Fistulas are usually perianal and up to 50% of patients may end up with an anal abscess (9). They are classified by their relation to the sphincter mechanism and usually fall under five anatomic categories i) superficial, ii) intersphincteric, iii) transsphincteric, iv) suprasphincteric and v) extrasphincteric as described by Parks in 1976 (10). Diagnosis and detection of fistula route is the key for proper management of treatment. Fistulography was the first method used to visualise anal fistulas. Further advancements in diagnostic imaging led to significant improvements in tackling fistula cases and namely these are the Three-Dimensional Endoanal Ultrasound (3-DEU) and Magnetic Resonance Imaging (MRI). Nevertheless, these technologies still have numerous limitations which are described elsewhere (11, 12). Perianal fistulas are considered as a big challenge for the surgeons, because of the existing wide variety of treatment methods result in a wide range of success rates. Therefore, the accurate identification of the correct path of fistula in the preoperative process is crucial to ensure optimal surgical treatment.
Herein, we demonstrate the implementation of a 3D printed pre-operative model to replicate and visualise an anorectal fistula as an attempt to properly recognise and identify its route. 3D printed replicas of anal fistulas mimic the mechanical properties of live human tissue, making them ideal for improved preoperative planning, and also potentially as an excellent tool for surgical training.
Ten patients (n=10) were admitted to our general surgery department with anorectal fistula disease. Patients underwent a full clinical examination and Magnetic Resonance Imaging (MRI). MRI images were taken with 1.5. Tesla to get the maximum possible resolution for our final models. Complex fistula lesions (like Rectovaginal fistulas and Horshoe fistulas) and patients with inflammatory bowel disease were excluded from the study. The MRI sequence that was used to display and generate the 3D model of the fistulae included sagittal T2 at the pelvis level, a coronal oblique STIR and T1 post gadolinium to the anal canal. Free CAD software (©google sketchup), has been used to digitally render a three-dimensional (3D) model of a patient’s anal fistula anatomy using MRI data. After isolating the relevant structures in each image set, 3D volume reconstruction was performed. Final model was saved in the .STL format (Figure 1a) that supports the visualisation of the model with a fully rotated virtual 3D representation (360° on the x, y and z axes). A printed model of the processed 3D digital model was created by a 3D printer (©MakerBot) using red and black polylactic acid (PLA) filament material with a diameter of 1.7.5 mm, while the layer thickness of the printed object (Figure 1b) was 0.1. mm. Scanning electron microscopy (SEM) has been used to characterize the 3D-printed object layer thickness, otherwise known as the printer’s resolution (Figure 2). Physical pre-operative models of the processed 3D digital models were created by a 3D printer with the mean fabrication time of 138 min, which is less as compared to fistula tract complexity. The cost of each model was in the range of 3¢ considering the price of the ABS filament and the weight of the material used. Cost of the 3D printer (©MakerBot printer) was 2500$, and for this study an already installed printer in our experimental laboratory was used. The low cost of our experimental study, give us the opportunity to train surgeons in visualizing the anatomy in different surgical fields in a cost-efficient manner.
 Figure 1
Figure 1A-B. A representative 3-D digital (a) and printed (b) model of fistula used for 3-D printing. Each model resulted from the respective MRI sequences and appropriate 3-D reconstruction process.
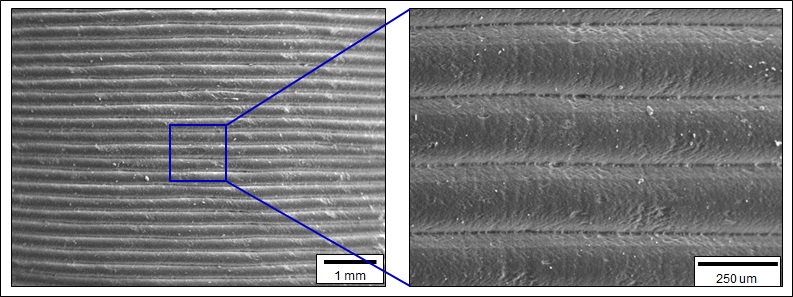 Figure 2
Figure 2SEM images of a 3-D printed object cross section depicting the layer thickness.
No personal information was collected. The study was approved by the Investigational Review Board (IRB) of the Aristotle University, Thessaloniki, Greece. Moreover; all methods were carried out in compliance with the relevant guidelines and regulations. Written informed consent was obtained from all patients, which was approved by the hospital Scientific Council. All presented results are in accordance with the approved guidelines.
A random controlled trial was designed to compare 3D printing models and MRI imaging regarding their efficiency as a tool to identify anal fistula routes. A total number of twenty (n=20) resident surgeons in the last year of their residency, were randomly divided into two groups in separate rooms. In the first group (group A), residents (n=10) had 15 minutes to review 2D MRI images, whereas in the second independent group, (group B), residents (n=10) reviewed only the 3D printed models. Both groups then completed a preoperative assessment test on the evaluation of anal fistula disease. A questionnaire was designed for this evaluation (tab1). Finally, all patients were operated upon by same colorectal team surgeons. After surgery, the colorectal team surgeons evaluated the assessment test of resident surgeons in both groups (group A, group B) and compared them to their operative findings. A flow chart of the study design is shown in Figure 3.
| Category of question | Group A (n=10); Median (IQR) | Group B (n=10); Median (IQR) | P | |
|---|---|---|---|---|
| Q1 | Imaging findings | 73 (63-82) | 87,5 (83-92) | 0.1.93 |
| Q2 | Location and compared with adjacent | 69 (59-80) | 85 (81-93) | 0.0.06 |
| Q3 | Fistula route Sphincter mechanism involvement | 69,5 (60-77) | 88,5 (84-94) | 0.0.08 |
| Q4 | Sphincter anatomy | 74 (64-80) | 89 (85-95) | 0.5.74 |
| Q5 | Sphincter mechanism involvement | 78,5 (71-82) | 92,5 (90-97) | 0.1.81 |
| Q6 | Correlation with St Marks proforma | 72,5 (61-77) | 90,5 (88-94) | 0.0.59 |
| Q7 | Important structures identification | 78,5 (70-84) | 92,5 (89-97) | 0.6.74 |
| Q8 | Characterization of primary and secondary track | 76,5 (71-82) | 90 (87-93) | 0.9.84 |
| Q9 | Evaluation of pelvic disease | 85,5 (80-90) | 69 (60-73) | 0.8.32 |
| Q10 | Preoperative planning | 71,5 (69-78) | 81 (79-88) | 0.0.01 |
| Overall mean score | 74,85 (66,8-73,5) | 87,2 (82,6-91,6) | ||
| N: number of subjects, P: Probability value, Q: Question category, IQR: Interquartile range | ||||
 Figure 3
Figure 3Flow chart of study design.
Continuous variables were expressed as the median and categorical variables as a number (%). P-value<0,05 was of significance. Statistical analysis was performed with IBM SPSS version 22 (IBM Corp, Armonk, NY). Categorical variables were compared with chi-squared test, while the comparison of the answers between group A and B was performed with paired samples T-test and Kolmogorov-Smirnov test.
An example of an anal fistula model is shown in Figure 1. This example is a suprasphincteric anal fistula with the internal mouth at 6 o’clock, with the fistula exiting at 5 o’ clock and finally piercing the perineum at 6 o’ clock (external opening). More specifically, as it can be seen Zone A represents the internal sphincter muscle, Zone B represents the external sphincter and Zone C represents the puborectalis muscle. The internal opening is marked by a blue arrow and the external opening by a yellow one. The other models were constructed in the same way.
Scanning Electron Microscopy (SEM) images of a 3D printed pre-operative model cross section at two different magnified levels are shown in Figure 2. Low magnification is shown on the left-hand side and high magnification on the right hand-side. As it can be observed, the layer thickness of the object is in the range of 250 μm, which is comparable to the resolution of the MakerBot 3D printer manufacturer’s technical specifications. The layers of the printed object are the main feature of the 3D printing technology, which creates an object via the successive addition of layers.
Resident surgeons of both groups analysed all ten patients and the attending colorectal surgeons subsequently evaluated the resident surgeon’s test. The questionnaire of the anal fistula assessment test and the median % scores of their answers for each question category are shown in tab1. Statistical analysis of the surgeon’s answers is done with the Kolmogorov – Smirnov test, was proof of a normal distribution (P>0.0.5).
Resident surgeons who studied only the anal fistula 3D printed models, (Group B) achieved a higher overall score in the fistula assessment test (87,2 (82,6-91,6)) in comparison to resident surgeons (Group A) who studied only MRI images (74,85 (66,8-73,5)). To compare the answers of groups A and B, a paired samples T-test comparison was performed for each category of question. Residents in Group B, which used the 3D printed models, had a higher score in the questions having to do with imaging findings (Q1, p=0.1.93) and anatomical questions about sphincter anatomy (Q4, p=0.5.74), structure identification (Q7, p=0.6.74) and primary truck characterization (Q8, p=0.9.84). The evaluation of pelvic disease is difficult because we used hard and opaque material in our printing methods (Q9, p=0.8.32). The evaluation score is better for Group A answers but, there were no significant differences of score between the two groups. Although, Group B achieved better scores for the evaluation of the fistula route (Q2, p=0.0.06 and Q3, p=0.0.08) with a statistically significant trend. The most important finding of this study is that Group B achieved better scores in pre-operative planning (Q10, p=0.0.01) and higher correlation with St Mark’s Hospital form (Q6, p=0.0.5). The answers of the resident surgeons (X axis % score, Y axis category of question) were shown in a Box-Plot Graph (Figure 4). Questions, categories and scores for both groups were also shown (tab1). Another fact (Figure 4) is that the standard deviation of the scores in group B is smaller, possibly because of the accumulated knowledge from the use of the 3D printed models.
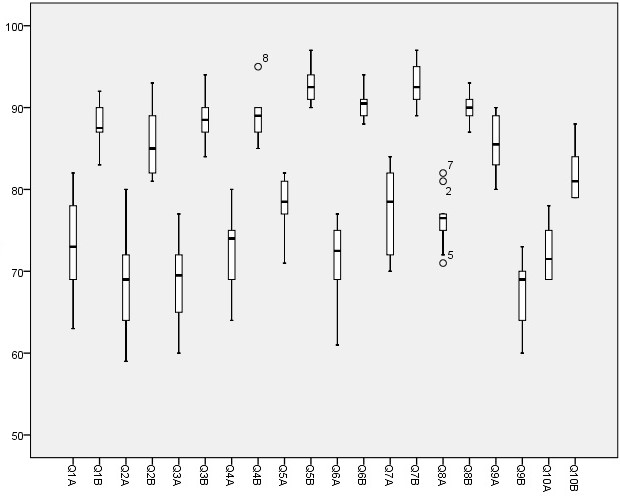 Figure 4
Figure 4Answers of young surgeons (X axis % score, Y axis category of question) were shown in Box-Plot Graph.
The questionnaire was used to evaluate the ease of learning between the two groups and with these different diagnosis tools. The questions were about: 1. Enjoyment, 2. Learning efficiency, 3. Authenticity of the methods, 4. Usefulness, 5. Ethics, 6. Intention to use and 7. Total satisfaction. The answers are between 1. (Strongly disagree) and 5. (Strongly agree).
Both groups were satisfied with the study and positive about the use of 3D printing technology for educational purposes. Almost all surgeons consider the fact that the learning goals have been achieved giving rise to successful handling of future anal fistulae disease surgeons. However, it is apparent that Group B surgeons have given in total much more positive answers (Figure 5a-c). Furthermore, participating surgeons noted that 3D models improved their preoperative awareness of the anal fistula and could use 3-D anal fistula model during the operation with the patient in the lithotomy position.
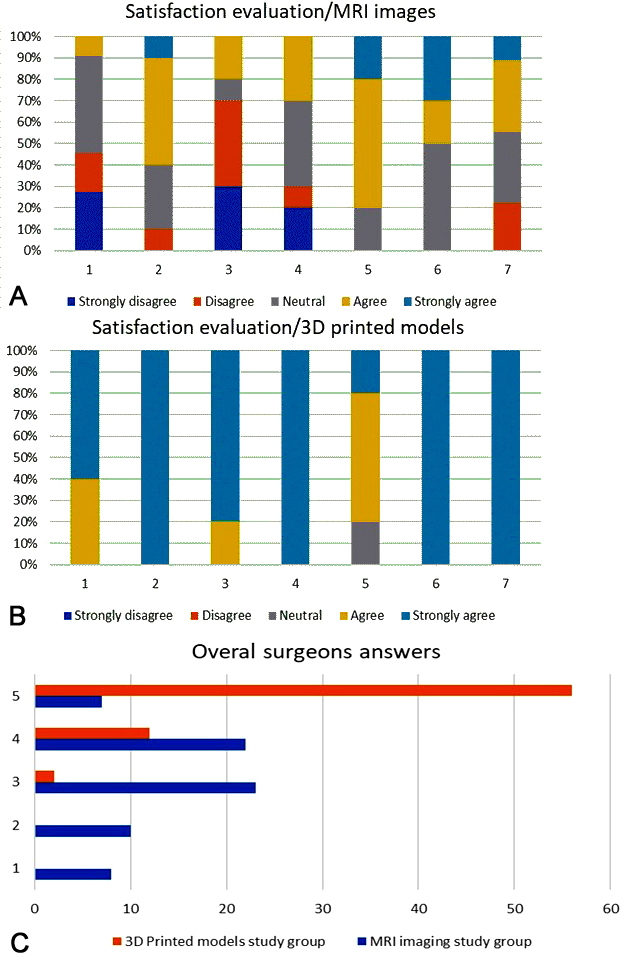 Figure 5
Figure 5A-B. Surgeons answers between Group A (Surgeons who study MRI images) and Group B (Surgeons who study 3D printed models). Questions were about: 1. Enjoyment, 2. Learning efficiency, 3. Authenticity of the methods, 4. Usefulness, 5. Ethics, 6. Intention to use and 7. Total satisfaction. The answers are between 1. (Strongly disagree) and 5. (Strongly agree). C. Overall surgeons satisfaction rates diagrams between Group A (Surgeons who study MRI images-Blue line) and Group B (Surgeons who study 3D printed models-Red line).
3D printed models have clearly demonstrated the exact anatomy of the anal fistula tract and its relationship to the surrounding sphincter mechanism. In addition, 3D printed models revealed the specific characteristics of the fistulae anatomy including size, configuration and exact route. The anatomy of the fistula tract is crucial in the preoperative planning as it will guide the selection of the best surgical treatment. Misdiagnosis of fistula tracts can lead to treatment failure and fistula recurrence. The classic assessment of fistula disease includes clinical examination, preoperative magnetic resonance imaging, three dimensional endoanal ultrasound and examination under anaesthesia (13). Knowledge of pelvic floor anatomy is essential.
Many studies have compared Ultrasound (US) and Magnetic resonance imaging (MRI) findings in the evaluation of anal fistulae. Both methods provide satisfactory accuracy, although MRI is frequently superior (12). Enhancement with H2O2 and gadolinium has been shown to be helpful with both techniques, especially in difficult cases (14). The type of fistula also plays an important role in selecting the appropriate method. The aim of surgery is to eradicate the anal fistulas, while at the same time preserving the sphincter function with the minimal sphincteric damage. The final treatment choice depends on the location of the anal fistula, the presence of sepsis and the clinical examination findings. For simple superficial fistulas, fistulotomy or fistulectomy is a sufficient treatment whereas, more complex fistulas like transphincteric or supralevator require more technically demanding procedures, such as seton suture, to avoid sphincteric segmentation and resulting incontinence. There are a lot of surgical techniques for the fistula treatment however, the experience of the surgeon and the initial assessment are crucial (9). MRI of the pelvis is the imaging tool of choice. MRI is also useful for fistulas associated with Crohn disease, although in the case of perianal abscesses and complexes fistulas such as those with horshoe routes, diagnostic accuracy is decreased, and negative false results are possible (15). There has been some discussion about the optimal MRI sequences, as reported elsewhere (16). In our patients, we used sagittal T2 imaging at the level of the pelvis, a coronal oblique short inversion time inversion recovery sequences (STIR) and a T1 post gadolinium image in the anal canal sequences. The STIR technique was superior to the fat-saturated MR imaging. The MRI images were performed using a 1.5. Tesla unit system after intravenous automatic injection of a gadolinium-based agent. The duration of the scan for all sequences was about 15-30 min (17).
The method used by St Mark's Hospital, which is based on the Parks classification, is a reliable method for the determination of the course of the fistula tract. St James University hospital classification is more detailed than St Mark’s and it is based on MRI findings, even though the latest classification is more complex without verification of the intraoperative findings (15). Rapid prototyping is an innovative technology that allows the construction of an anatomically correct 3D model of a patient. There have been many studies on the implementation of 3D printing technology in several surgical fields including orthopaedics, cardiovascular, maxillofacial for educational and preoperative purposes (13). In the last decade (2005-2015), 1067 papers were published evaluating the role of 3D printing in surgery. These studies stem from 37 different, mostly highly technologically developed countries such as China, Germany, United States, Japan, and the UK. Most of references concerning advantages of 3D printing (48.7%) are related to the improvement of planning the surgical procedure, thanks to the visualization, simulation and better understanding of the procedure. Another 25.3% refers to the production of surgical materials, 9.5% discusses implant construction and 6.3% facial prostheses (18). Our present study is the first application of 3D printing technology in the field of coloproctology. 3D printed anal fistula models were used in surgical education, planning, training, and spatial anatomy configuration. In our study, the 3D models allowed resident surgeons to touch, manipulate and explore the relationship of the fistula tract to the surrounding sphincter structures prior to the operation. According to the anal fistula assessment test results, we believe that the quality of preoperative planning is improved when young surgeons can learn, improved planning and training on a 3D model simulation. This enhances surgical skills and improves patient safety in the operating theatre.
Our replicas allowed the resident surgeons to visualize and understand the entire fistula tract thus enhancing the perception of the spatial anatomy. Total cost of our method is quite low considering the advantages for both the pre-surgery planning, as well as the educational importance for young surgeons. The cost of a specific Fused Deposition Modelling (FDM) 3-D printer which is in the range of 2500 € and printing a single model costs 3-5 €. Low cost is important as it can have significant impact in developing countries, where the one-time investment of the printer can help to train the caregivers. This type of personalized patient-based training and surgical care fistulas allows the management of more difficult fistula cases, while ensuring the safety of the patient. The prototyping method is safe, non-invasive and requires only the standard MRI imaging of the pelvis. Our original study is clinical and focuses on anatomically simple fistulae. It could be expected that the benefit of prototyping would be greater in anatomically complex cases. Future studies will be concentrating on the development of automation software modelling for the pelvic floor anatomy. This would allow physicians to generate models in-house to guide customization of anal fistula without external resources. Our study has a possible limitation in the pelvic floor disease while 3D printing material was opaque and hard. Transparent and flexible filament materials will be used in our future studies that may be better suited for the surgical training purposes (19). Next generation 3D printers and new type of printing materials, can give us more abilities to training a lot of caregivers in many fields of surgery.
Petros Bangeas, Kostantinos Drevelegkas, Christina Agorastou, Lazaros Tzounis, Aggeliki Chorti, and Daniel Paramythiotis, were responsible for the diagnosis and treatment of the patients and assisted in the preparation of the manuscript. Antonis Michalopoulos, Vassileios Papadopoulos, George Tsoulfas, Aristomenis Exadaktylos and Jasjit Suri, assisted in the preparation of the manuscript and provided useful insights. All authors, would like to gratefully acknowledge the International Centre for Excellence in Emergency Medicine Bern/Swiss and Bodossaki foundation. Authors have no conflicts of interest or financial relationships to disclosure.
Key Words: Anal Fistula, Resident Training, 3D Printing, Surgical Education, Preoperative Planning
