Academic Editor: Paolo Casadio
Background: Given that total laparoscopic hysterectomy (TLH) is less
invasive than open surgery, its popularity has increased in Japan. The aim of the
present study was to determine the most appropriate uterine size for the safe
completion of TLH for the treatment of uterine leiomyomas. Methods: This
retrospective study included 505 patients who underwent TLH for uterine
leiomyomas. Patients were divided into three groups according to the weight of
the excised uterus (
Uterine leiomyomas are benign monoclonal tumors affecting the smooth muscle cells of the myometrium, comprising a large amount of extracellular matrix containing collagen, fibronectin, and proteoglycan [1, 2]. Leiomyomas grow in 80% of women and can cause exhaustion symptoms such as heavy, irregular, and prolonged uterine bleeding; anemia; bulk symptoms (e.g., pelvic pressure/pain, obstructive symptoms) and fertility issues. Myomas affect different races differently: Myoma-related symptoms are more common in African American women, who often exhibit higher numbers of leiomyomas with larger uteri, which may increase the incidence of complications or blood transfusion requirements when compared with rates observed in Caucasian women [3, 4, 5]. Medical management using hormone-based preparations (e.g., oral contraceptives, levonorgestrel containing intrauterine system (IUSs), and gonadotropin releasing hormone (GnRH) agonists) is possible in patients with symptomatic uterine myomas [6]. While these therapies provide varying degrees of control in patients with abnormal uterine bleeding, most do not act directly on the myomas. Thus, surgical intervention remains the mainstay of uterine leiomyoma treatment.
In the United States, more than 250,000 hysterectomies are performed annually for the treatment of myoma only [7]. Medical and surgical treatment of leiomyomas can negatively influence the reproductive system, causing significant morbidity and decreasing quality of life [8, 9], and leiomyomas can relapse after non-hysterectomy treatment. The parameters of surgical treatment for these tumors depend on their size and location. When compared with open surgery, total laparoscopic hysterectomies (TLHs) are less invasive, having gradually obtained acceptance as an alternative approach to tumor excision in Japan due to decreased blood loss and shorter hospital stays [10]. TLHs have been the subject of significant controversy, however, especially in patients with a large uterus. Previous reports have considered uterine sizes in patients beyond 12 weeks of gestation or greater than 280 g large [11, 12]. These large uteri are frequently associated with an increased risk of complications and morbidities, such as intraoperative bleeding, postoperative complications, and longer hospital stays following TLH [13]. On the other hand, some have also suggested that TLH is preferable to other surgical approaches in patients with enlarged uteri undergoing total abdominal hysterectomy [14, 15].
The present study aimed to evaluate the association between uterine size and complications in patients with leiomyoma who had undergone TLH between 2014 and 2021 at Shimane Medical University hospital. We sought to determine the uterine size for which the TLH approach is most effective in these patients.
This study was conducted in the Department of Obstetrics and Gynecology at Shimane Medical University Hospital in Japan. The study included 505 patients who underwent TLH between July 2014 and December 2021. All patients had benign indications for TLH such as abnormal uterine bleeding, pelvic pain, fibroid uterus, and endometriosis. All operations were performed by a resident physician under the supervision of an attending physician. All patients underwent physical examination including pelvic ultrasonography, blood tests, and a detailed evaluation of clinical history. Patients were hospitalized the day before surgery. All patients provided written informed consent for laparoscopic surgery. This work was authorized by the Institutional Review Board of Shimane University (IRB no. 201912120-1).
Patient groups were defined according to uterine weight following excision on
pathological examination: Group A included patients with a uterine weight
Student’s t-test was used to compare data among the three groups.
p-values
Data were analyzed for a total of 505 patients who had undergone TLH for benign
conditions. The median ages of patients in group A (uterine weight
| Variable | Group A (n = 347) | Group B (n = 125) | Group C (n = 33) | p values | ||
| Uterus |
Uterus 500–1000 g | Uterus |
A vs. B | A vs. C | B vs. C | |
| Age, years | 47.9 (28–82) | 46.3 (32–63) | 47.4 (34–55) | 0.204 | 0.149 | 0.473 |
| Total myoma weight, g | 254.9 (41–499.5) | 686.4 (500–993) | 1278.8 (1000–2000) | 0.000 | 0.000 | 0.000 |
| Bleeding volume, mL | 116 (10–1000) | 208 (10–2060) | 402 (10–3500) | 0.005 | 0.015 | 0.099 |
| Surgical duration, min | 163.3 (231–242) | 190.3 (106–408) | 209 (106–453) | 0.005 | 0.005 | 0.058 |
Mean intraoperative blood loss was significantly lower in group A (mean: 116 m; range: 10–1000 mL) than in group B (mean: 208 mL; range: 10–2060 mL) or C (mean: 402 mL; range: 10–3500 mL). No significant differences in blood loss were observed between groups B and C (Fig. 1, Table 1). Mean surgical duration was significantly shorter in group A (mean: 163 min; range: 231–242 min) than in group B (mean: 190 min; range: 106–408 min) or C (mean: 209 min; range: 106–453 min). No significant differences in surgical duration were observed between groups B and C (Fig. 2, Table 1). MR imaging revealed that enlarged uteri weighing over 500 g extended beyond the sacral promontory. However, in patients with uteri under 500 g, a hypointense area was observed anterior to the sacral promontory (Fig. 3). Representative pathological images of excised uteri for the three groups are presented in Fig. 4.
 Fig. 1.
Fig. 1.Blood loss further stratified by uterine weight.
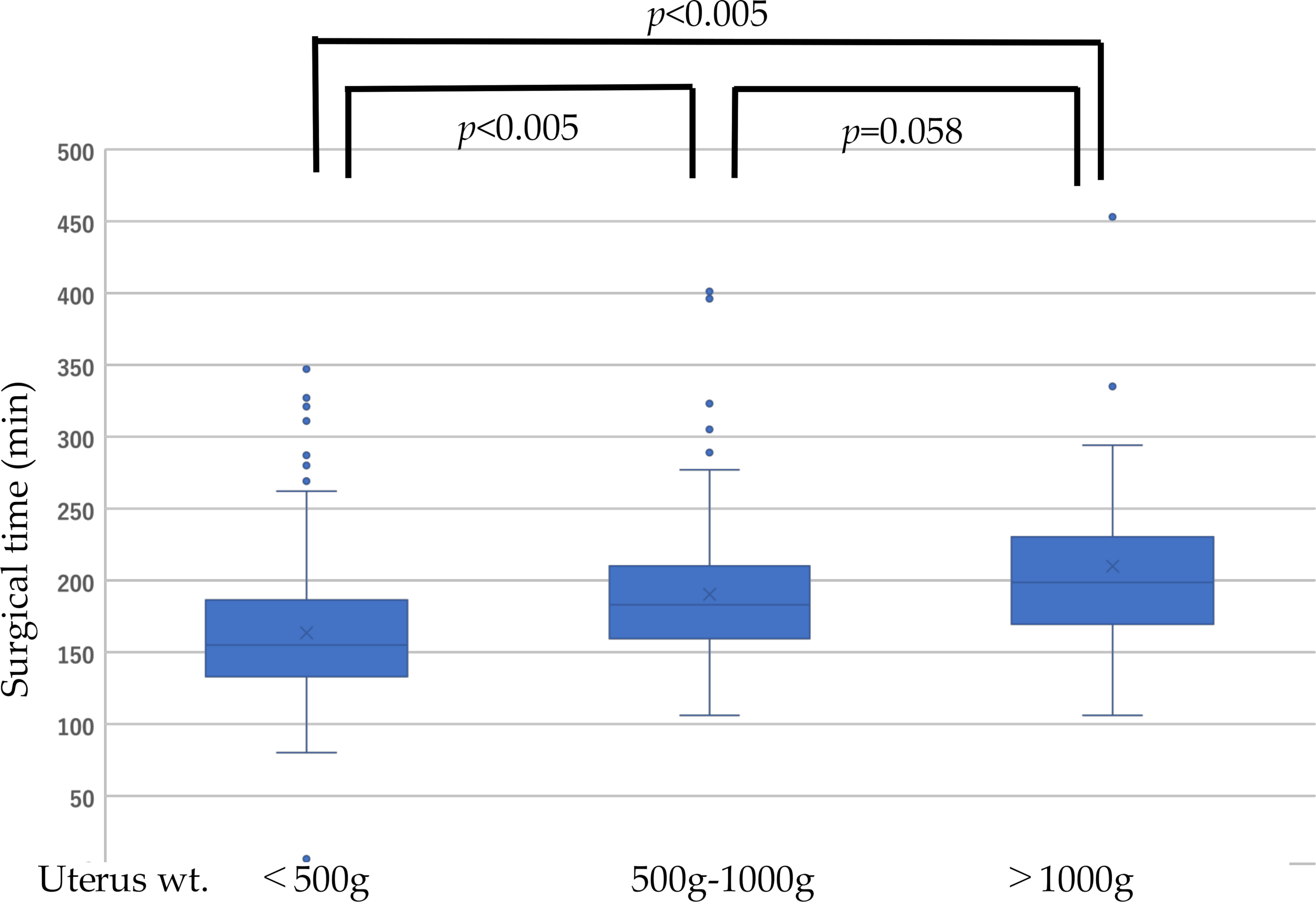 Fig. 2.
Fig. 2.Surgical duration further stratified by uterine weight.
 Fig. 3.
Fig. 3.MRI comparison. (a) MRI image showed that myoma wt more than 500g restricted inside the sacral promontary. (b) more than 500 g extended beyond the sacral promontary .
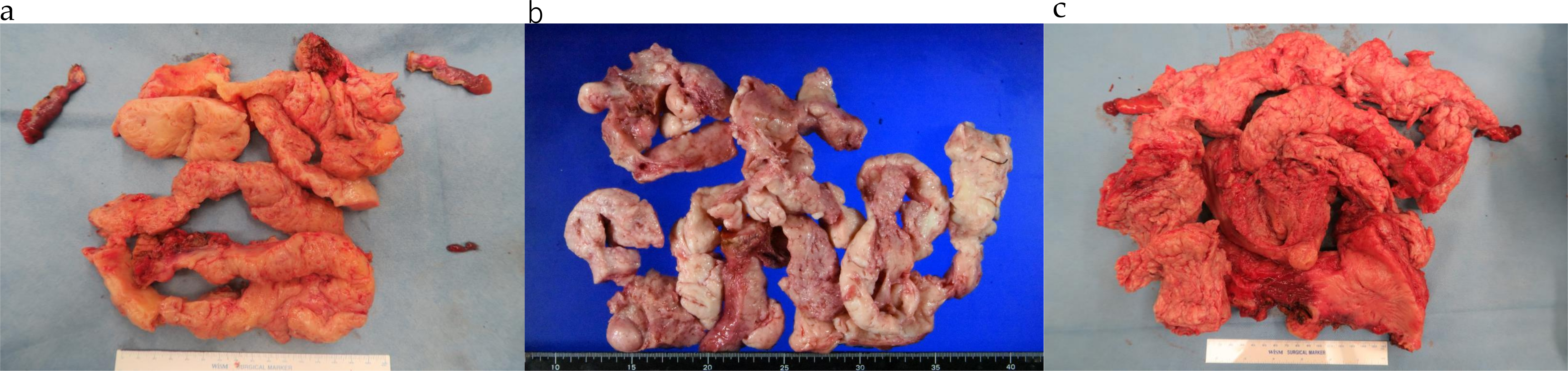 Fig. 4.
Fig. 4.Representative images of uterine myomas weighing. (a) 440 g, (b) 960 g, and (c)1960 g following pathological examination.
Uterine leiomyomas are the most common tumors arising from the female reproductive tract. These tumors slowly increase in size, and treatment is considered when their presence is associated with certain symptoms such as hypermenorrhea, abdominal pain, abdominal distension, and infertility.
Technological advances continue to revolutionize the surgical treatment of gynecologic conditions. Innovations in minimally invasive surgery for TLH were first documented by Reich et al. [16], since which their application has increased in Japan. However, TLH should be performed by experienced surgeons to avoid complications, such as injury to the bladder and rectum [17, 18, 19]. TLH was initiated in our department in 2014 and has been carried out since then as a standardized procedure. The amount of time needed for this surgery has decreased in recent years as the number of TLH cases has increased. Prior work has demonstrated that TLH reduces the length of hospitalization, the volume of blood loss, surgical duration, and rates of rare complications regardless of uterine weight [10]. Surgeons may experience difficulties and potential risk when handling cases with enlarged uteri, which can limit the operative field and prolong procedure time. No specific guidelines have provided standardized limitations related to TLH based on uterine size. Although hypogastric artery ligation has been found to reduce blood loss in more complex laparoscopic hysterectomy [20] but this technique is still challenging.
In the current study, we investigated the relationship between uterine weight
and surgical outcomes including postoperative bleeding and operation time. Median
operating time as well as blood loss varied based on uterine weight, and the
smallest uteri (
Taken with previous findings, the current results indicate that uterine weights
These data suggest that TLH is ideal when an individual patient’s uterine weight
is
The present study demonstrated that TLH can be performed safely by resident
physicians when the uterine size is
TI, SR, KN drafted the manuscript. HY, MI, and SS collected data; TI performed statistical analysis; KN participated in this study; SK participated in coordinating this study. All authors read and approved the final manuscript.
All patients provided written informed consent for laparoscopic surgery. This work was authorized by the Institutional Review Board of Shimane University (IRB no. 201912120-1).
Not applicable.
This research received no external funding.
The authors declare no conflict of interest. KN is serving as one of the Guest editors of this journal. We declare that KN had no involvement in the peer review of this article and has no access to information regarding its peer review. Full responsibility for the editorial process for this article was delegated to PC.
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
