†These authors contributed equally.
Academic Editor: Paolo Ivo Cavoretto
Background: Cervical insufficiency, or cervical incompetence, describes the condition in which the cervix dilates without painful uterine contractions in the second trimester of pregnancy. It often leads to loss of pregnancy or preterm delivery. Recommendations for the prophylactic placement of cervical sutures are well established, however rescue cervical cerclage for a prolapsing amniotic bag is more controversial due to higher technical demands, higher risk of iatrogenic rupture of membranes, and questionable long-term neonatal prognosis. This study aimed to answer two important questions: (1) Should rescue cerclage be performed for those with an evidently protruding amniotic bag? (2) Who would benefit the most from rescue cerclage? Materials: Eighteen pregnant women with cervical incompetence with a clinically evident prolapsing amniotic bag from January 2016 to February 2020 were included. Four received conservative treatment, i.e., without cerclage, and the other 14 patients opted to receive emergency rescue cervical cerclage. Results: We classified the patients into futile (n = 7) and successful (n = 7) cerclage groups at post-operative day 21. Pregnancy and neonatal outcomes were obviously better in the success group, however no significant pre-operative predictive factors for success could be identified. The results of the women who did not receive cerclage and those with futile cerclage were comparable. Rescue cerclage was especially beneficial for those at 22 weeks to 26 weeks of gestation. Conclusions: The maternal and fetal outcomes of the patients with futile rescue cerclage were comparable to those who did not receive cerclage. Therefore, rescue cerclage for advanced cervical insufficiency could be considered, especially for those at 22 weeks to 26 weeks of gestation.
Cervical insufficiency, or cervical incompetence, describes the condition in which the cervix dilates without painful uterine contractions in the second trimester of pregnancy. It often leads to loss of pregnancy or preterm delivery. The diagnosis is confirmed based on findings of a protruding amniotic bag or dilated cervix in sonography or a vaginal speculum examination. Recommendations for the prophylactic placement of cervical sutures for women (1) with previous cervical insufficiency, (2) having previously had one or more spontaneous pregnancy losses in the second trimester, and (3) with a history of preterm delivery before 34 weeks of gestation, and presenting with a short cervix (less than 2.5 cm before 24 weeks of gestation) in sonography in this pregnancy are well established due to the obvious prolongation of pregnancy and favorable outcomes after cerclage [1, 2]. Nonetheless, placing rescue cervical cerclage for a prolapsing amniotic bag is more controversial due to higher technical demands, higher risk of iatrogenic rupture of membranes, and questionable long-term neonatal prognosis [1, 2, 3, 4]. Even if rescue cerclage is performed smoothly without rupture of membranes, the dilated cervix, protruding amniotic bag, and foreign cervical sutures still predispose women to rupture of membranes, chorioamnionitis, and preterm labor. The efficacy or clinical benefits of performing such a high-risk procedure is therefore controversial.
There are still no firm recommendation regarding rescue cerclage due to the lack of powerful randomized controlled trials. However, observational cohort studies suggest beneficial clinical outcomes after rescue cerclage [5, 6, 7, 8, 9, 10, 11]. A meta-analysis conducted by Ehsanipoor et al. [5] included 10 studies and reported significantly increased neonatal survival (relative risk of 1.65) and prolongation of pregnancy (mean difference of 34 days) in those undergoing rescue cerclage compared to expectant management. Similarly, Abu Hashim et al. [12] reported a 2-fold reduction in preterm delivery before a gestational age of 34 weeks in their review article. However, some obstetricians and patients still hesitate over the use of rescue cerclage, mainly over concerns of iatrogenic rupture of membranes and chorioamnionitis, which can cause severe maternal and neonatal complications. Consequently, more studies on the use of rescue cerclage are needed.
The current study is a retrospective analysis of cases collected over 4 years. We focused on women with a prolapsing amniotic bag beyond the outlet of the cervix rather than those with a dilated cervical inlet noted in sonography only. Pregnancy and neonatal outcomes were analyzed and discussed. This study aimed to answer two important questions: (1) Should rescue cerclage be performed for those with an evidently protruding amniotic bag? (2) Who would benefit the most from rescue cerclage?
This retrospective study was approved by the Institutional Review Board (IRB) of Kaohsiung Medical University Hospital (KMUHIRB-E(I)-20200190). Pregnant women with cervical incompetence with a clinically evident prolapsing amniotic bag and who were treated at Kaohsiung Medical University Hospital from January 2016 to February 2020 were included. Based on their presenting conditions with or without active bleeding, regular uterine contractions or apparent infectious signs, shared decision-making of whether or not to perform rescue cervical cerclage was conducted among the patients, family and attending obstetricians. Patient characteristics including age, parity, body mass index, gestation number, gestational age at surgery and at delivery, infection parameters, fever or not, cervical dilatation, size of the protruding bag, newborn body weight, Apgar scores, and mortality rates were collected. All operations were performed by an experienced senior obstetrician.
At admission, the patients underwent history taking, laboratory studies, fetal sonography (Fig. 1A), speculum examination (Fig. 1B), and tocodynamometry. Cervical cultures were collected in the lower genital tract. Rescue cerclage was performed under epidural anesthesia. Pre-operatively, prophylactic antibiotics were given, the bladder was emptied, and the vulva and vagina were sterilized with betadine solution, and then rinsed quickly with sterile saline to avoid irritation to the fragile amniotic membranes. In the Trendelenburg position, the operation started by reducing the protruding amniotic bag slowly and carefully with a large rinsed cotton swab until the effaced cervix could be visualized. A 16-French foley catheter was inserted into the uterine cavity with a balloon and gradually inflated while retrieving the cotton swab. The cervix was then grasped with Allis forceps at 0, 3, 6 and 9 o’clock positions. The McDonald suture was performed with one or two Mersilene tapes at the operator’s discretion (Fig. 2). The intrauterine Foley catheter was carefully deflated and removed while tying the tape(s).
 Fig. 1.
Fig. 1.Diagnosis of cervical insufficiency. (A) Transabdominal sonography finding of a prolapsed amniotic sac. (B) Speculum examination of cervical insufficiency.
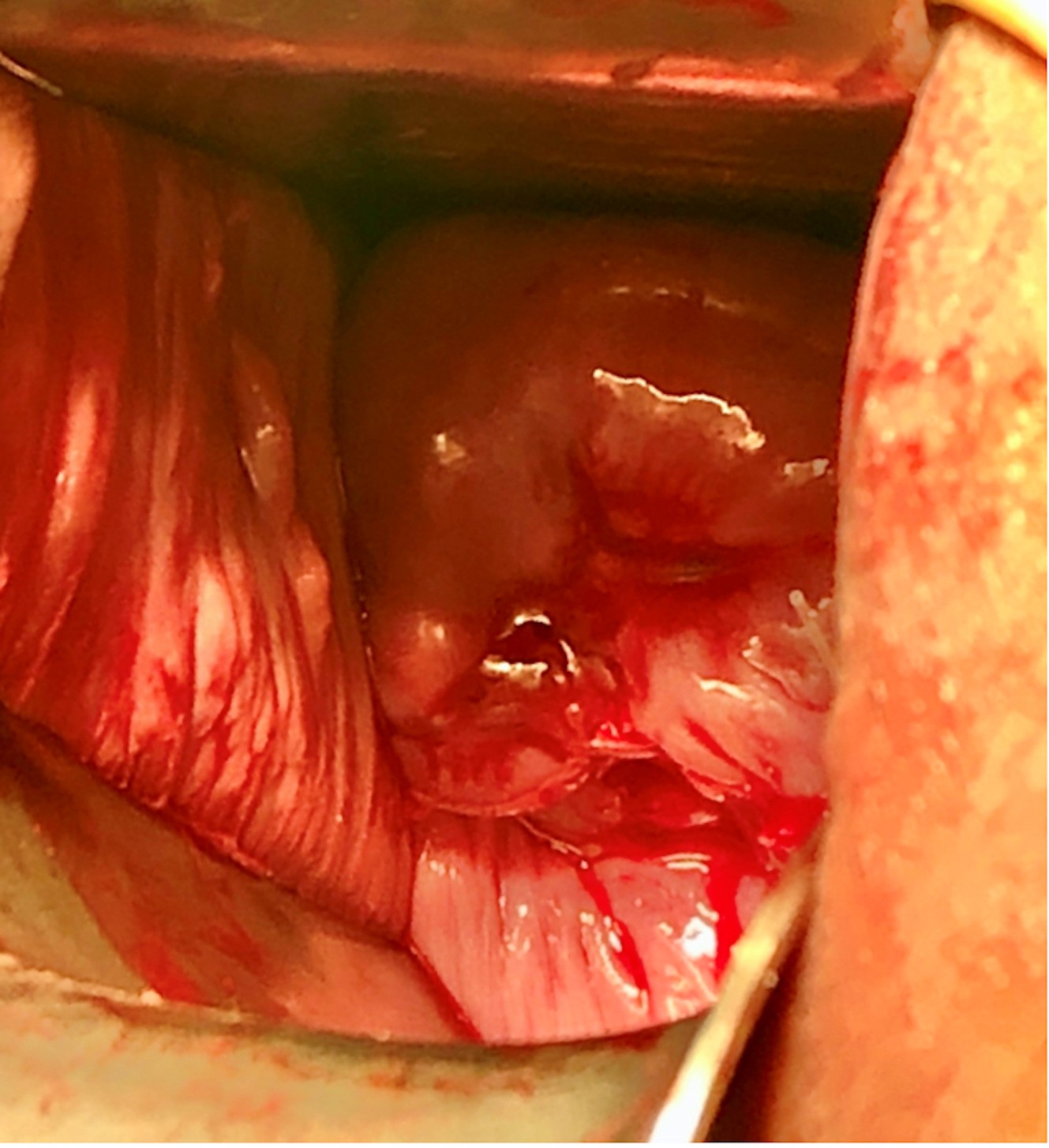 Fig. 2.
Fig. 2.Speculum examination after reducing the amniotic sac and cerclage insertion for the same patient in Fig. 1.
After the operation, the patient was required to remain quietly in bed with the Foley catheter indwelling. Tocolytic medications with progesterone (weekly intramuscular injections), calcium channel blockers, non-steroidal anti-inflammatory drugs, and beta mimetics were given when regular uterine contractions were detected by tocodynamometry or the patient’s subjective feelings. Empirical antibiotics with second-generation cephalosporins were given and adjusted afterwards according to microbiological culture and antibiotic sensitivity reports. Weekly laboratory studies were done to detect evident chorioamnionitis. We shifted to the oral form of antibiotics after the first 7 days after rescue cerclage if there were no obvious signs of infection. Fetal well-being was assessed by continuously monitoring the fetus. Betamethasone for fetal lung maturity and 48-hour magnesium sulfate for fetal neuroprotection were given when delivery was expected within the next 7 days. The cerclages were removed when spontaneous rupture of membranes occurred, active labor ensued with bloody show, uncontrolled uterine contractions occurred and non-reassuring fetal heart beat patterns were noted.
The women who declined rescue cerclage received comparable non-invasive medical management, including cervical swab, empirical antibiotics with second-generation cephalosporins, 17 alpha-hydroxyprogesterone caproate and tocolytic medications (e.g., beta mimetics, and calcium channel blockers). Newborn outcomes including birth body weight, Apgar scores at the first and fifth minutes, and survival rates were collected.
Statistical analyses were performed using SPSS version 22 (IBM Corporation,
Armonk, NY, USA). The level of significance for all tests was p
Eighteen women were included in the present study. Four received conservative management without any surgical intervention, one of whom had twin pregnancy. The other 14 patients opted to receive emergency rescue cervical cerclage, of whom three had twin pregnancies (Table 1). None had abandoned surgical attempts. On post-cerclage day 21, the percentage of undelivered women reached the first plateau, and no one delivered in the following 17 consecutive days (Fig. 3). Therefore, we used a cutoff value of 21 days to define futile cerclage and successful cerclage. According to this definition, seven women had prolonged pregnancy for 21 days or more and were considered to have a successful cerclage outcome, and seven women delivered within 21 days and were considered to have futile cerclage. One of the seven futile cases had rupture of membranes during surgery.
| No cerclage | Cerclage | p value | |||
| (n = 4) | Futile (n = 7) | Success (n = 7) | |||
| Age (years) | 24 |
35.9 |
31.6 |
0.186 | |
| BMI (kg/m |
28.5 |
30.1 |
23.7 |
0.093 | |
| Parity (Nulliparous/Multiparous) | 2/2 | 4/3 | 7/0 | 0.051 | |
| Twin pregnancy (Yes/No) | 1/3 | 1/6 | 2/5 | 0.5 | |
| Fever ( |
0 | 0 | 0 | ||
| WBC at admission (/uL) | 11,110 |
12,914 |
9902 |
0.051 | |
| CRP level (mg/L) | 6.9 |
25.6 |
11 |
0.423 | |
| Protruding bag (cm, by PV) | 5.5 |
4.3 |
4.8 |
0.346 | |
| OP interval (hours) | - | 19.3 |
20.8 |
0.930 | |
| GA at admission (weeks) | 21.6 |
21.0 |
23.8 |
0.074 | |
| GA at delivery (weeks) | 22.3 |
22.5 |
33.6 |
||
| GA interval (days) | 5 |
10.3 |
68.7 |
||
| Foley (Yes/No) | 1/3 | 2/5 | 6/1 | 0.031* | |
| Maternal outcome | |||||
| Chorioamnionitis | 0 | 0 | 0 | ||
| Postpartum hemorrhage | 0 | 0 | 0 | ||
| Neonatal outcome | |||||
| Birth body weight (grams) | 544 |
525 |
2060 |
||
| Discharge alive (Yes/No) | 2/2 | 1/6 | 7/0 | 0.001* | |
| Take-home babies | 3 | 1 | 9 | ||
| (1 pair of twins) | (2 pairs of twins) | ||||
| Babies without major morbidity | 1 | 1 | 9 | ||
* p value with statistical significance when compared between the cerclage/futile and cerclage/success groups. Abbreviations: BMI, body mass index; WBC, white blood cells; CRP, C-reactive protein; PV, per vaginal examination; OP, operation; GA, gestational age. | |||||
 Fig. 3.
Fig. 3.Comparison of tocolysis duration and cumulative number of undelivered women between no-cerclage and cerclage groups. A plateau at 21 days after surgery significantly differentiated those with early delivery and those with a prolonged pregnancy.
The mean age of the women who did not receive cerclage (N = 4) was 24
For those with futile cerclage (N = 7), the average maternal age was 35.9
With regards to the successful cerclage group (N = 7), the average maternal age
was 31.6
These results showed that pregnancy status became more stable after the pregnancy had been prolonged for more than 21 days, and also that the neonatal survival rates dramatically increased. Besides survival rate, neonatal morbidity was another important outcome. Babies in the successful cerclage group had no sequelae, while those in the other two groups, i.e., conservative and futile cerclage groups, still required long-term rehabilitation or treatment to some degree. Detailed data are presented in Table 1.
Statistical analysis revealed no significant difference in pregnancy outcomes or newborn survival between the no-cerclage group and futile cerclage group (p = 0.993). However, significant differences were observed between the no-cerclage group and successful cerclage group in tocolysis duration, gestational age at delivery, newborn body weight, and newborn survival rate. Similarly, the successful cerclage group had significantly superior clinical outcomes with regards to gestational age at delivery, tocolysis duration, newborn body weight, and newborn survival rate (Fig. 4). They also had significantly longer bed rest and Foley catheter indwelling time. No significant differences were found in the degree of leukocytosis at admission, parity, interval between admission and surgery, or gestational age at admission between the futile and successful cerclage groups. We did not routinely measure C-reactive protein, a common marker of infection. Microbiological reports are shown in Table 2. There was no predominant species in either group.
| Futile Group | N = 7 | Success Group | N = 7 |
| Bacteroides fragilis | 2 | Bacteroides fragilis | 1 |
| E. coli | 1 | E. coli | 1 |
| Lactobacillus crispatus | 1 | Lactobacillus crispatus | 1 |
| Acinetobacter baumannii complex | 1 | Lactobacillus gasseri | 1 |
| Streptococcus mitis | 1 | Streptococcus agalactiae | 1 |
| Bifidobacterium dentium | 1 | Enterococcus faecalis | 1 |
| Morganella morganii ssp morganii | 1 | Klebsiella pneumonia ssp ozaenae | 1 |
| Citrobacter koseri | 1 |
 Fig. 4.
Fig. 4.Intervals between admission and delivery. The neonatal survival
rates were 0%, 60%, 100% at a gestational age of
In this study, the success rate of rescue cerclage, arbitrarily defined as pregnancy prolongation more than 3 weeks, was around 50%, and the pregnancy and neonatal outcomes were promising. The survival and take-home baby rates were good, and no significant neurologic sequelae were noted. With regards to the 50% cerclage failure rate, both maternal and neonatal outcomes were comparable to those who received conservative management. Whether or not to receive rescue cerclage is a difficult decision for the women and their families. They face an impending loss of pregnancy if they do nothing, but are still at high risk of iatrogenic premature rupture of membranes if they receive rescue cerclage. This is an important issue, and especially for older women and infertile couples.
A similar take-home baby rate was reported by Gundabattula’s group in 2013 [13]. Zhu et al. [11] reported a success rate of 82.3% in their analysis of 158 patients, and Shivani et al. [10] reported a live birth rate of 92.5% in 6-year study using comparable surgical techniques and tocolytic management. The variations in reported live birth rates could be partially related to different inclusion criteria.
Vaisbuch et al. [14] reported a 3-week diagnosis-to-delivery interval in asymptomatic pregnant women with a cervical length of 0 mm revealed in sonography in the second trimester managed expectantly. In the current study, the diagnosis-to-delivery interval was only about 5–7 days in those who were treated conservatively. This may suggest that a prolapsing amniotic bag beyond the cervix represents a more severe type of cervical incompetence than a short cervical length only. In this study, spontaneous rupture of membranes and delivery in those who received cerclage occurred until a marked plateau at around 21 days post rescue cerclage, after which the rates decreased (Fig. 3). Subclinical infection, which cannot be clinically detected, is one of the most common causes of spontaneous rupture of membranes. Our results suggest that a 3-week observation period seems to be sufficient to rule out subclinical infection.
We used post-operative day 21 as the cutoff point to dichotomize favorable pregnancy outcomes from futile rescue cerclage in an attempt to determine the predictive factors of successful rescue cerclage. Even though none of the factors achieved significance, which may be due to the small sample size, a younger maternal age, primipara, less leukocytosis, and older gestational age on admission were favorable factors. We did not perform cerclage in those with remarkable signs of infection or painful uterine contractions. Leukocytosis is an obvious indicator of active infection, and it has been associated with a failure to prolong pregnancy in previous reports [11, 15, 16, 17]. In addition, white blood cell count is also influenced by pregnancy itself [18, 19], and a correlation between the number of leukocytes and ongoing labor course has been reported [20]. At what level white blood cell count is predictive of futile cerclage remains unknown, and further investigations are needed to clarify this issue. There were no significant differences in C-reactive protein level and body temperature between the futile and success groups in this study. Details of the bacteria cultured from cervical swabs are listed in Table 2. There was a large variation between individuals, which made it difficult to define a correlation between the microbiological environment and cerclage success rate. A gestational age on admission of more than 22 weeks seemed to play a role, and was associated with better success rates (Fig. 4) of neonatal survival and rescue cerclage.
The prolongation of pregnancy was especially beneficial for those with a
gestational age of 22 weeks to 26 weeks. A recent executive summary published
from multiple associations stated that a previable birth is considered as
delivery taking place from a gestational age of 20 0/7 weeks to 25 6/7 weeks
[21]. Extremely preterm is defined as delivery before 28 weeks of gestation.
Neurodevelopmental impairment is very common among these infants. A systematic
review reported a progressive decrease in the incidence of moderate-to-severe
neurodevelopmental impairment among newborns who survived at 4–8 years of
follow-up with each week gained in gestational age at delivery: 43% at 22 weeks,
40% at 23 weeks, 28% at 24 weeks, and 24% at 25 weeks of gestation [22]. In
our study, the overall survival rates were 0%, 60% and 100% for those
delivered at
Practice guidelines recommend the use of 17 alpha-hydroxyprogesterone caproate in women with previous preterm birth history, and vaginal natural progesterone in those with an asymptomatic shortening cervix [15, 16]. We used weekly intramuscular injections of 17 alpha-hydroxyprogesterone caproate in our tocolysis protocol. Although current evidence and practice guidelines discourage the routine use of antibiotics in spontaneous preterm labor [17, 23], empirical antibiotics were prescribed in our tocolysis protocol because our high-risk patients were prone to chorioamnionitis with the loss of cervical barriers. Second-generation cephalosporins were used empirically, which were then adjusted according to cervical swab culture results and antibiotic sensitivity tests. If no sign of infection was identified or noted, we shifted the antibiotics to an oral form of first-generation cephalosporins after the first 7 days post cerclage. None of these women developed clinical chorioamnionitis during postpartum follow-up. Further studies are required to justify the prolonged use of antibiotics in this particular high-risk group.
We did not perform amnioreduction prior to rescue cerclage, as it could lead to herniation of amniotic membranes from the cervix after successful cerclage. It is possible that reducing intra-amniotic bag pressure may decrease the risk of iatrogenic rupture of membranes during cerclage. Amniocentesis is also a risk factor for chorioamnionitis and stimulus of uterine contractions. Cakiroglu et al. [24] reported comparable results between groups with or without amnioreduction before rescue cerclage. Other than intra-amniotic bag pressure, the effectiveness of anesthesia can also influence the risk of rupture of membranes. Suboptimal anesthesia can lead to the patient feeling pain and involuntarily fighting against it, which can then result in increasing intra-abdominal pressure and rupture of membranes.
We found that prolonged bed rest with the Foley catheter indwelling significantly contributed to the success rate of rescue cerclage (p = 0.031). This may be due to decreased ambulation between the bed and bathroom, reduced postural change and movement, and consequently reduced abdominal pressure. Most current evidence advises against unselective prolonged best rest or physical restriction as a means to prevent preterm delivery. A Cochrane review in 2015 by Sosa et al. [25] found no evidence either to support or refute this advice. An updated systematic review and meta-analysis reported by Matenchuk [26] even suggested worse newborn outcomes in women suffering from complicated pregnancies with more than 1 week of bed rest in developed regions. However, this evidence included high-risk pregnancies with increased risks of preterm delivery without subgroup analysis of those receiving rescue cerclage. Few studies on rescue cerclage have included subgroup analysis on the efficacy of post-operative physical restriction. Risks associated with prolonged bed rest, particularly thromboembolism [27, 28], are recognized and addressed in patient counselling. In-bed leg exercises, massage, compression stockings, and coordinated care by rehabilitation specialists have been recommended to reduce relevant complications. Our study is limited by the relatively small number of cases. Ethical issues and shared decision making on treatment options make randomized controlled trials impossible. More and better designed studies are needed to make further solid recommendations.
Rescue cerclage is emerging as a recommended technique in patients with physically diagnosed cervical incompetence. It is also helpful for those with an advanced protruding amniotic sac. In this study, the clinical outcomes were markedly improved if the surgery was successful and if the pregnancy was prolonged beyond 3 weeks after surgery. The maternal and fetal outcomes of the futile rescue cerclage group were comparable to those who did not receive cerclage. In addition, the neonatal survival rate improved dramatically and the incidence of comorbidities decreased if the delivery occurred after 24 weeks of gestation. Therefore, rescue cerclage for advanced cervical insufficiency could be considered, especially for those at 22 weeks to 26 weeks of gestation. Although some studies have reported that C-reactive protein, leukocytosis and microbiological assessment are preoperative prognostic factors, no specific factor was identified to predict successful cerclage in the present study. In our case series, post-operative bed rest with the Foley catheter indwelling was helpful in prolonging the pregnancy without noticeably increasing the incidence of thromboembolism. Further studies are needed to make more solid recommendations.
TFC designed the research study. CRK, ILH and SHW performed the research and analyzed the data. CRK and WYH wrote the manuscript. All authors contributed to editorial changes and amendment in the manuscript. All authors read and approved the final manuscript.
This is a retrospective study with protocols approved by the Institutional Review Board (IRB) of Kaohsiung Medical University Hospital (KMUHIRB-E(I)-20200190). Pregnant women suffering from cervical incompetence with clinically evident prolapsed amniotic bag cared at KMUH from January 2016 to February 2020 were included.
All individuals who helped in this study are appreciated. We are especially grateful for the supporting from Kaohsiung Medical University Hospital.
The work was supported by Kaohsiung Medical University Research foundation (KMUH 108-8R43, KMUH 109-9R43, KMUH-11010, KMU-TC108A04-0, KMUH-S11007).
The authors declare no conflict of interest. TFC is serving as one of the Guest editors of this journal. We declare that TFC had no involvement in the peer review of this article and has no access to information regarding its peer review. Full responsibility for the editorial process for this article was delegated to PIC.
Publisher’s Note: IMR Press stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
