† These authors contributed equally.
Background: Spontaneous perforation of pyometra is a rare clinical emergency with high mortality. As pyometra perforation is difficult to recognize pre-operatively, many cases are mis-diagnosed as gastrointestinal (GI) rupture. This study aimed to develop a strategy to improve diagnostic accuracy of spontaneous uterine perforation in female patients with acute abdomen. Methods: Twenty-two women with spontaneous rupture of the uterus (twenty cases previously reported in the literature plus two cases from the authors’ hospital) were included in the study group, another 22 menopausal patients with GI perforation were selected as the control group. Radiologists carefully reviewed the CT images and reports and summarized some common signs in patients with spontaneous perforation of pyometra. GI patients’ CT images were also scrutinized for these characteristic signs. The occurrence of these features was calculated in both groups. All patients underwent abdominal surgical exploration and most of patients diagnosed with spontaneous perforation of pyometra received hysterectomy and bilateral oophorectomy. Results: Five characteristics were specifically detected in patients with uterine spontaneous perforation: (1) Fluid collected in the cul-de-sac, incidence 95.5%; (2) Fluid in the uterine cavity, incidence 100%; (3) Intra-uterine free air, incidence 90.9%; (4) Free air around the uterus, incidence 77.2%; (5) Defects on the uterine wall, incidence 72.7%. However, these five signs were rarely observed in control patients with GI perforation. A dignostic strategy combined clinical findings with raidiological features were developed to help identify these patients. Conclusions: The above five CT characteristics and the developed dignostic algorithm could be used as a tool to facilitate the preoperative diagnosis of spontaneous perforation of pyometra, although more tests are needed in large samples of cases.
Pyometra is common in elderly females secondary to the infection of the endometrium, especially in developing countries. The reported incidence in postmenopausal women is about 0.2%, while it is infrequent in the premenopausal female. The two most common factors leading to the disease are trauma or malignant diseases occurring in the cervix, and congenital anomalies of the genital tract. On very rare occasions, pyometra can develop spontaneous perforation, presenting as acute abdomen. Without immediate and specific treatment, septic shock may occur and patients are at great risk of mortality. Therefore, early identification is extremely important for patients with spontaneous perforation of pyometra. Unfortunately, many of these patients are misdiagnosed at an early stage with gastrointestinal perforation, which results in referral to general surgeons. During the ensuing emergency surgeries, improper upper abdominal exploratory incisions are made, wasting a large amount of time in checking for non-existent stomach and bowel lesions.
This paper evaluated the clinical and imaging material of 22 cases of spontaneous perforation of pyometra. From our analysis, five computer tomography (CT) characteristics were unique in this disease and could be used to facilitate pre-operative diagnosis of spontaneous perforation of pyometra with improved accuracy.
We searched in PubMed with the keywords “spontaneous perforation”, “spontaneous rupture” and “pyometra”, “uterus”; only English language articles published between 1972 to 2018 were included. Fifty-four case reports and series were found. From these, 20 cases with satisfactory pelvic CT images or detailed descriptions were included in our study. In addition, another 2 cases from the authors’ hospital were also incorporated. In total, 22 cases were subjected to our analysis.
Another 22 menopausal women with gastrointestinal perforation from the authors’ hospital were included as a control group, so that the characteristic signs in uterine rupture patients could be assessed.
The CT images or image descriptions of 20 cases from the cited reports and the two cases from the authors’ hospitals were analysed; the image features are described and summarized in Fig. 1. All the medical materials from the two authors’ cases were also comprehensively analysed and reviewed, and are presented in Figs. 2,3. All of the CT image review was done by two independent radiologists. After this review, several CT characteristics [Two common signs: (1) ascites or abdominal fluid; (2) pneumoperitonium or subdiagphratic free air and five featured signs: (1) intrauterine fluid; (2) intrauterine air; (3) free air around the uterus; (4) defects in the uterine wall; (5) fluid in the cul-de-sac] became the focus of assessment.
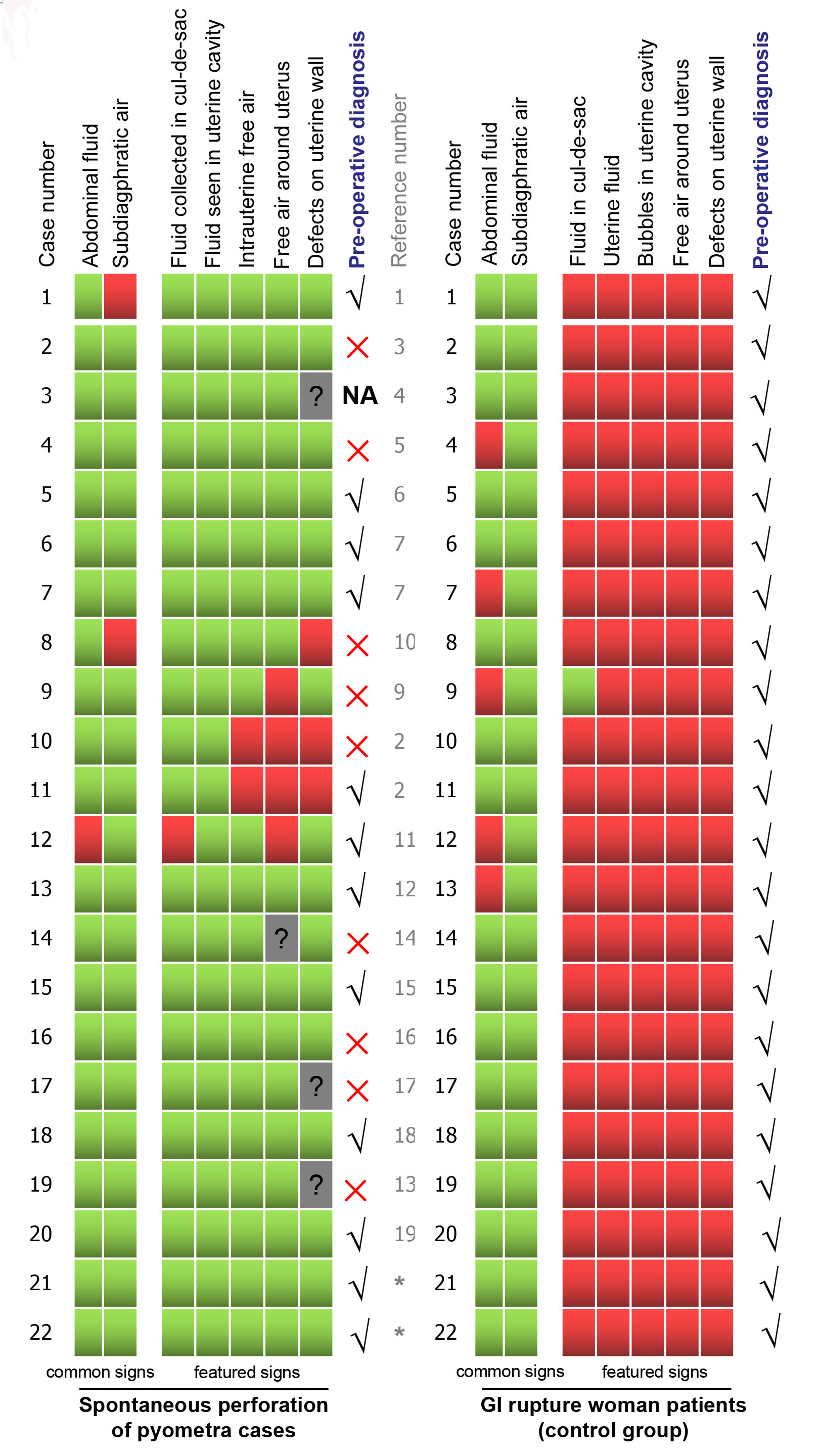 Fig. 1.
Fig. 1.Summary of CT characteristics in both uterine and GI rupture patients. Two common and five featured CT signs in individuals from both groups are listed in this figure. The green colour means the specific sign was present in the patient’s CT images; the red colour means the specific sign was absent from either evaluation of patient’s images or the description in the report; the grey colour with an interrogation mark means the information cannot be obtained from the available material. √ shows the patients’ preoperative diagnosis was right, × indicates the preoperative diagnosis was incorrect.
 Fig. 2.
Fig. 2.Representative CT images of 5 featured signs in spontaneous perforation of pyometra. This figure presents CT images of two cases from the authors’ hospital. The five representative CT features for spontaneous perforation women are listed. These are “Intrauterine fluid” & “defects on uterine wall” (arrow, A,B), “Intra-uterine free air” (arrow, C,D), “free air around uterus” (arrow, E,F), “fluid in cul-de-sac” (arrow, G,H).
 Fig. 3.
Fig. 3.Gross pathology in two cases of spontaneous perforation of pyometra. The four pictures show pus within the uterine cavities and perforating locations which penetrate the posterior uterine walls (A,B).
“Fluid-filled uterus” was defined as liquid material with different density observed in the uterine cavity. “Intrauterine free air” was diagnosed when gas could be detected within the uterine cavity. “Free air around the uterus” was a common sign when air was distributed adjacent to the uterine body. “Defect in the uterine wall” indicated filling-defects within the myometrium of the uterine body. “Fluid in the cul-de-sac” meant fluid had collected in rectovaginal pouch.
Fig. 1 lists the imaging characteristics of the 22 uterine rupture cases [1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19]. All of these patients except one were menopausal women, with a median age of 70, ranging from 40 to 90 years. Acute abdominal pain was noted in almost all cases, and it also presented as the chief complaint while coming to the emergency department.
Similar to common imaging findings in the perforation of other hollow viscus, 21 uterine rupture patients had abdominal fluids, with fluid collected around the liver and spleen (Fig. 1). Twenty patients (90.1%) had pneumoperitonium, or subdiagphratic free air (Fig. 1). Similar findings were also observed in the control group, the cohort of 22 gastrointestinal perforation patients, with abdominal fluid around the liver and spleen in 17 cases (77.2%). Subdiagphratic free air was noted in all these patients (100%) (Fig. 1).
Five CT signs were frequently observed in uterine perforation patients, while none of them could been detected in GI perforation cases. These were uterine fluid (22 patients, 100%, Fig. 1, Fig. 2A,B), intrauterine free air (20 patients, 90.1%, Fig. 1, Fig. 2C,D), free air around the uterus (17 patients, 77.3%, Fig. 1, Fig. 2E,F), defect in the uterine wall (16 patients, 72.7%, Fig. 1, Fig. 2A,B), fluid collected in the cul-de-sac (21 patients, 95.5%, Fig. 1, Fig. 2G,H). After thorough examination of the GI perforation CT images, only very few of the above five signs were noted (Fig. 1).
The gross pathology of the perforated uteruses of the two patients at our hospital are shown, with spontaneous perforated wounds due to muscle inflammatory necrosis. Massive pus was filled in and around the uterus and distributed over the whole peritoneal cavity from the penetrating holes (Figs. 3,4).
 Fig. 4.
Fig. 4.Graphic summary of the five CT characteristics in patients of spontaneous perforation of pyometra.
As indicated above, the difference in incidence of pyometra between premenopausal and postmenopausal women can be attributed to various causes. Older women with years of atrophy of their female genital tract tend to have cervical stenosis; fluid may then accumulate. When bacterial infection occurs, an abscess is formed within the uterine cavity with no outlet. Perforation and acute abdomen may then result in these postmenopausal patients. Premenopausal women, in whom genital tract atrophy rarely occurs, only suffer uterine rupture when natural drainage of the tract is compromised by some disease, such as cervical cancer. Very few uterine rupture cases with cervical cancer have been reported. There were less than 10 cervical cancer patients with spontaneous pyometra perforation reported in the English-language literature. All of these cases were not accurately recognized preoperatively.
Despite differences, similar uterine CT features facilitating the diagnosis of spontaneous perforation of pyometra have been raised in some case reports [3, 7]. Physicians have indicated 3 key findings of uterine perforation: (1) presence of fluid in the uterus, (2) defect of the uterine wall, (3) intraperitoneal fluid connecting to the intrauterine fluid. Unfortunately, there has been no subsequent evidence to support this diagnostic strategy. This current report, to the best of our knowledge, may be the first analysis to summarize the CT features of uterine spontaneous perforation.
The principal findings of our study are as follows. First, five specific CT signs were identified among women with spontaneous perforation of pyometra. Second, the five CT signs, mostly specific for uterine perforation and rarely detected in GI perforation cases, could be implemented as a diagnostic algorithm. In this study, we assessed twenty-two cases with images of both CT and gross specimens. From these cases, uterine free air and free air around the uterus were detected in 89.5% and 84.2% of patients, respectively. The two CT signs are of great value in assisting diagnosis and have been repeatedly emphasized by other clinicians [20, 21]. This makes biological sense, as evidence shows that most of pathogens causing pyometra include anaerobes or some aerobes, which were generally aerogenic [22, 23, 24, 25, 26].
A retrospective review suggests that implementing these five CT characteristics to assist diagnosis would have considerable usefulness. Where these features have been recognized before surgery, diagnosis accuracy was improved significantly. Twelve of the 22 cases (54.5%) in the current study were correctly diagnosed before operation. Within the correctly diagnosed 12 patients, 10 cases (83.3%) embraced all the five features in their CT images, 1 (8.35%) bore 3 features, and the other 1 (8.35%) had 2 features. Notably, according to a previous study, preoperative diagnostic accuracy was only 13.6% before CT technology was commonly used [27].
Fluid collected in the cul-de-sac was also a specific manifestation in uterine perforation patients, as shown in previous published cases. In both of the authors’ two cases, redundant pelvic fluid was observed. However, in control GI perforation women, although 77.2% of patients (17/22) had abdominal fluid around the liver and spleen, only one of them (1/22, 4.5%) had fluid collection in the cul-de-sac, because of massive leakage of GI content.
The five CT characteristics (Fig. 4) would be useful for clinicians, as some frequently noted signs, such as a systemic inflammatory response, acute abdomen signs and pneumoperitonium, or subdiagphratic free air, usually have little value for differential diagnosis. For physicians, when encountering elderly women with acute abdomen, the five features in CT images would assist them to distinguish perforation of uterus from GI injuries.
Our study, to the best of our knowledge, may be the first report to summarize specific criteria to identify spontaneous perforation of pyometra. The use of this strategy might facilitate preoperative diagnosis of the disease, although further prospective studies were needed. As only 22 cases had CT images available for analysis, studies recruiting more uterine spontaneous perforation patients should be conducted.
Other limitations were as follows: First, we included relatively few clinical cases available for analysis, because it is a rare disease with low incidence. Second, as the incidence is even lower in premenopausal women, we have no premenopausal cases included as a control group for CT feature analysis. In addition, lack of pyometra patients without perforation as the control counterparts is also a problem. However, as these patients usually have no acute abdomen symptoms, it is not difficult to distinguish in clinical practice. Furthermore, the CT images for analysis were limited, so probably some important information could have been omitted.
In conclusion, we highlight five CT characteristics (Fig. 4): (1) Fluid collected in the cul-de-sac; (2) Fluid in the uterine cavity; (3) Intra-uterine free air; (4) Free air around the uterus; (5) Defects on the uterine wall that may facilitate the preoperative diagnosis of spontaneous perforation of pyometra. Based on this finding, we developed a diagnostic strategy for women with spontaneous perforation of pyometra. The potential patients must first meet at least two of the three essential criteria. When conformed, doctors may refer to the elaborate criteria which the increased matching items enhance the diagnostic accuracy (Table 1).
| Essential criteria | |
| Acute abdominal Pain, Abdominal tenderness | |
| Abdominal fluid or Pneumoperitoneum | |
| Fluid seen in uterine cavity | |
| Elaborate criteria | |
| Fluid collected in cul-de-sac | |
| Intrauterine free air | |
| Free air around uterus | |
| Defects on uterine wall |
CT, computer tomography; GI, gastrointestinal.
Conceptualization: ZX, XGX. Data curation: YYH, CRL, FL. Formal Analysis: YYH, CRL, ZGS, YZC. Investigation: YYH, CRL, FL, JL, PLC, WWW. Project administration: ZX, XGX, JL, PLC, WWW. Resources: YYH, CRL, FL, ZX. Software: ZX, YYH, RM. Validation: ZX, XGX, YYH, CRL. Visualization: ZX, RM. Writing — original draft: YYH, CRL, FL, ZX. Writing — review & editing: ZX, XGX. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript.
Patients provided informed consent for publication of the cases and the study was approved by the ethics committee of the First Affiliated Hospital of Dalian Medical University, China. The ethics reference number is YJ-KY-FB-2020-56.
Not applicable.
This project was supported by Tibet Local Science and Technology Project guided by Central Government (Grant No. XZ202001YD0005C), Scientifical Funds of Medical Assistance Program for Tibet from Tibet Health Committee (Grant No. XZ2020ZR-ZY77(Z), Grant No. XZ2020ZR-ZY78(Z)), the Natural Science Funds of Liaoning (Grant No. 2019-BS-073), the Scientific Funds of Liaoning Education Department (Grant, LZ2019044).
The authors declare no conflict of interest.
