Background: To further understand Robert’s uterus and sum up the experience of diagnosis and treatment for Robert’s uterus. A 17-year-old woman came to our hospital for dysmenorrhea in 18 April 2012. She had had severe dysmenorrhea [VAS (visual analogue scales): 6 marks] since her menarche occurring in December 2010. Gynecological examination: patent vagina and a smooth cervix. Type-B ultrasonic instrument indicated two uterine cavities. The right uterine cavity contained a liquid anechoic area. There was no continuous echo between the right uterine inferior segment and cervical canal, and there was only a cervical echo. For further diagnosis and treatment, the patient underwent hysteroscopy combined with laparoscopy. The patient was diagnosed with Robert’s uterus and received removal of the uterine septum. Five years later, the patient smoothly gave a full-term baby boy. Conclusion: Gynaecologists must pay close attention to the primary dysmenorrhea occurring in juvenile females in order to find uterine malformation early as much as possible.
Robert’s uterus, a very rare uterine malformation, was first reported by Robert in 1970 [1]. There were only 43 articles about Robert’s uterus from 1970 to 2015 [2]. Robert’s uterus has a normal outside shape and is characterized by having a complete asymmetric oblique septum which divides the uterine cavity into an obstructed hemicavity and non-obstructed hemicavity. In order to provide a reference for diagnosis and treatment of Robert’s uterus, we report a patient who had Robert’s uterus and experienced a successful pregnancy after surgery performed by hysteroscopy combined with laparoscopy.
All study methods were approved by Institutional Review Board and Ethics Committee of Hubei Maternal and Child Health Hospital [(2020) IEC (lw047)]. The patient reported in this study gave written inform consent to participate.
A 17-year-old woman came to our hospital for dysmenorrhea in 18 April 2012. She was unmarried but had sexual life. Her menarche occurred in December 2010. She had menstruation once every 25–30 days and each menstruation lasted for 5 days, but menstrual volume was small and dysmenorrhea [VAS (visual analogue scales): 6 marks] was severe during menstrual onset. In February 2011, she received the removal of hematosalpinx and the right salpingostomy due to the right lower abdominal pain combined with pelvic mass in another hospital (the specific condition is not clear) after the third menstrual onset. After operation, her dysmenorrhea failed to be relieved and was aggravated (VAS: 8 marks), so she came to our hospital. In our hospital, she said that she had no sexual life for nearly six months. Type-B ultrasonic instrument suggested possible duplex uterus, blood accumulation in the right uterine cavity and a cystic mass in the right appendage area (suspected chocolate cyst). The patient was referred to our hospital on 16 May 2012.
Physical examination on admission: There was a 10-cm surgical scar in the middle of her lower abdomen.
Gynecological examination: Vulva was married and non-productive. Vagina was patent. She had a smooth cervix without lifting pain. Her uterus was anteflexed and widened with a size similar to a male fist. Her uterus was mobilizable and had marked tenderness. Bilateral appendages were not palpable.
Auxiliary examinations: Cancer antigen 125 (CA-125): 102 U/mL (normal range
Based on above examinations, the preliminary diagnoses were uterine malformation (rudimentary horn of uterus? Bicornuate uterus? Or Robert’s uterus?).
 Fig. 1.
Fig. 1.Unicornuate uterus with one oviduct opening. The hysteroscopy indicates narrow uterine cavity. The right uterine horn and oviduct opening are not seen. Note: The arrow indicates that there is only the left oviduct opening, which is in consistent with unicornuate uterus.
For definite diagnosis and further treatment, the patient underwent hysteroscopy
combined with laparoscopy on 23 May 2012. The laparoscopy showed that the
greater omentum widely adhered to the anterior abdominal wall. When the adhesion
was separated, a lot of chocolate-like fluid flowed out (Fig. 2). After
separating the adhesions, the uterus was clearly seen. The uterus widened and
seemed to contain two uterine bodies, but the uterine fundus was continuous. The
left uterine body was normal in size, but the right one obviously enlarged (Fig. 3). The right ovary was 4 cm
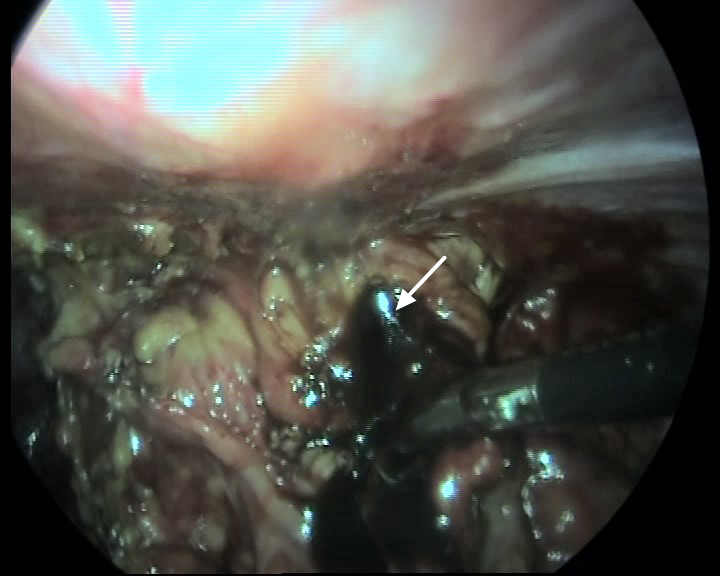 Fig. 2.
Fig. 2.Adhesions between the greater omentum and the anterior abdominal wall, as well as chocolate-like liquid. Notes: The arrow indicates chocolate-like liquid. After separating the adhesion between the greater omentum and the peritoneum, the chocolate-like liquid wrapped by the the greater omentum is seen.
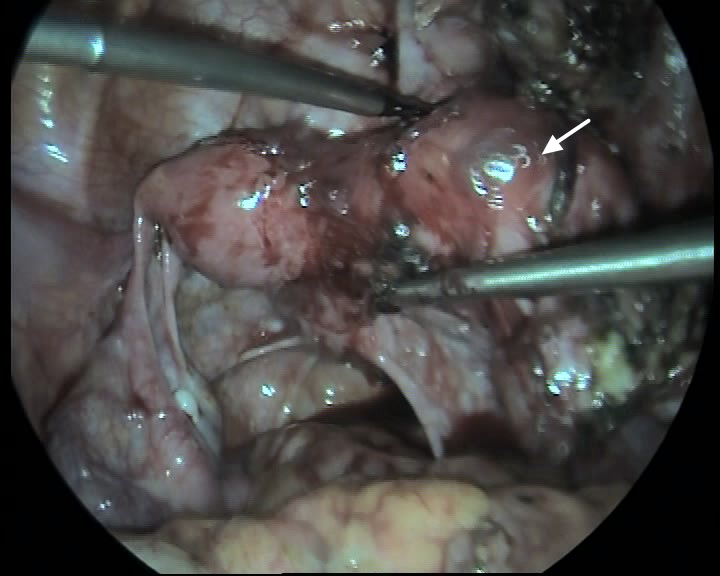 Fig. 3.
Fig. 3.Widened uterus with continuous uterine fundus.
Note: The arrow indicates the right uterus. The left uterine body is normal and the right uterine body is enlarged in size. The right uterine fundus is slightly
higher than the left uterine fundus, and there is a slight concave in the middle
between the left uterine fundus and right uterine fundus. The right ovary is 4 cm
Under laparoscope, methylene blue solution was injected into the right uterine cavity for guiding hysteroscope operation. After finding the oblique septum, the weak part of the oblique septum was cut using the hysteroscope monopole electrode needle, and then the methylene blue solution combined with coffee solution and brown tissue pieces flowed out. Under the guidance of type-B ultrasonic instrument, the oblique septum was completely removed. The right uterine cavity and the right oviduct opening were clearly visible, and the whole uterus returned to a shape of inverted triangle.
The patient was diagnosed with Robert’s uterus, pelvic endometriosis, right ovarian endometriosis cyst and right salpingitis by hysteroscopy, laparoscopy and pathology.
An intrauterine device was used to prevent uterine cavity adhesion one week after operation, and was removed 3 months after operation. At the same time, the patient took 4 mg of progynova once a day for 21 days, and took 20 mg of dydrogesterone after 11 days after operation for 10 days with a total of 3 cycles to avoid intrauterine adhesion.
The patient again received hysteroscopy 6 months after operation, and the morphology of uterine cavity was basically normal. In February 2017, the patient smoothly gave a full-term baby boy with a body weight of 3445 g by vaginal delivery.
The uterus originates from two Müllerian ducts which undergo development, fusion and septum absorption. Uterine malformation is closely related to the septum. In uterine malformation, mediastinal uterus is common, but oblique septum uterus is less. According to ESHRE-ESGE (European Society of Human Reproduction and Embryology-European Society for Gastrointestinal Endoscopy) classification [3], the uterine malformation in this study belonged to U2b. When the septum inclines to one side of the uterine cavity, the uterine cavity on this side is completely closed. Therefore, the menstrual blood can not flow out from the closed uterine cavity and the uterine cavity pressure gradually increases, resulting in severe abdominal pain. The symptoms vary according to different attachment points of the septum on the uterine wall [4].
Some scholars have summarized the characteristics of Robert’s uterus as follows: (1) primary dysmenorrhea; (2) different uterine appearances between laparoscopy and uterophotography; (3) no urinary system malformation [5]. In this study, the patient had primary dysmenorrhea. Type-B ultrasonic instrument indicated two uteruses, right pyometra and normal urology. The hysteroscopy displayed single cervix and the left oviduct opening; and after cutting open the oblique septum, hematocele in the right uterus was seen. The laparoscopy showed that the uterus widened and seemed to contain two uterine bodies, but the uterine fundus was continuous. Based on above findings, the patient was diagnosed with Robert’s uterus. In this patient, the accumulated blood in the right uterine cavity flowed out through the right fallopian tube into the right pelvic cavity, which led to right ovarian endometriosis cyst and increased CA-125 (102 U/mL).
The clinical manifestation of Robert’s uterus is very similar to rudimentary horn of uterus, so it is necessary to pay attention to their differential diagnoses. Before operation, it is difficult to definitely diagnose Robert’s uterus by two-dimensional ultrasound, three-dimensional ultrasound, hysterosalpingography, MRI, or even laparoscopy or hysteroscopy alone. Hysteroscopy combined with laparoscopy is the golden standard for the diagnosis and treatment of Robert’s uterus. If necessary, hysteroscopy and laparoscopy combined with B-ultrasound monitoring are used for the patients with atresic and narrow uterine cavity. In this patient, under laparoscope the outside shape of her uterus was normal; and the methylene blue solution was always not observed in the left uterine cavity after injecting methylene blue solution into the right uterine cavity, which suggested that there was no passage between the two uterine cavities. Therefore, the uterine malformation in this patient is consistent with the characteristics of Robert’s uterus; while in rudimentary horn of uterus and unicornuate uterus, their uterine fundus is separated.
Only surgery is effective for the treatment of Robert’s uterus. The traditional treatment for Robert’s uterus as the Strassmann’s metroplasty [6], is to open the uterus after laparotomy, remove the septum between the two uterine cavities, and then suture the two uterine bodies to make the two uterine cavities share the same cervix. Although laparotomy is a very effective method in the treatment of Robert’s uterus, it can cause damage to the uterine wall [7]. In the patient of this study, under the guidances of laparoscope and type-B ultrasonic instrument, the uterine oblique septum was removed using hysteroscope without damaging to myometrium, which reduced the risk of uterine rupture after pregnancy. With the development of ultrasonic diagnostic technology, ultrasonic monitoring can not only accurately measure the width and height of septum, but also guide accurate electroresection for removal of the septum [8].
According to postoperative thickness of septum and the degree of endometrial defect, Foley balloon or intrauterine device (IUD) should be placed in the uterine cavity, or estrogen-progesterone cycle treatment be used to assist endometrial repair and reduce intrauterine adhesion. It is recommended that the secondary hysteroscopy be performed after operation, and if there is residual septum, it should be resected [9]. For the patients with fertility requirements, pregnancy may be immediately carried out after endoscopic surgery, which shortens the time required by uterine wound repair after laparotomy [10].
Compared with the traditional laparotomy, hysteroscopy combined with laparoscopy can markedly relieve operation wound, and possesses some advantages such as minimally invasive, scar-free and fast postoperative recovery. Especially for the patients with fertility requirements, hysteroscopy combined with laparoscopy can retain the integrity of uterine muscle wall, which is beneficial to postoperative pregnancy.
Early and accurate diagnosis as well as appropriate surgical treatment are important for Robert’s uterus. Gynaecologists must be on guard against atypical obstructive Müllerian duct development malformation, and give close attention to the primary dysmenorrhea of the juvenile females in order to find uterine malformation early as much as possible [2].
During the operation, the injection of methylene blue solution into the atresic uterine cavity was used as a surgical guide to let we easily find out the septum. This is worth to be referred.
LZ and YY designed the research study. JD provided help and advice. LZ and YY provided and analyzed the data. LZ, JD and YY wrote the manuscript. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript.
All study methods were approved by Institutional Review Board and Ethics Committee of Hubei Maternal and Child Health Hospital [(2020) IEC (lw047)]. The patient reported in this study gave written inform consent to participate.
Thanks to all the peer reviewers for their opinions and suggestions.
This work was supported by the Open Research Fund Program of the State Key Laboratory of Virology of China (2021KF005).
The authors declare no conflict of interest.
