Pyometra is defined as the collection of purulent material in the uterine cavity. Colouterine fistula is a rare condition with less than 30 cases being reported in the literature. We believe this to be the first reported case of colouterine fistula secondary to pyometra. An 85-year-old woman with generalized abdominal pain and malodorous vaginal discharge for two weeks presented to the emergency room of Chonnam national university hospital. Physical examination confirmed the presence of the malodorous vaginal discharge. Abdominopelvic computed tomography scan demonstrated an abscess within the endometrial cavity and the presence of a fistula between the colon and the uterus. The patient underwent magnetic resonance imaging which revealed a communication between the distal sigmoid colon and the uterus. Total abdominal hysterectomy, bilateral salpingo-oophorectomy, drainage of the abscess and a sigmoid colon resection were performed. Histopathological study of the surgical specimen revealed acute suppurative inflammation without evidence of malignancy.
Pyometra is defined as the collection of purulent material in the uterine cavity [1]. It is a rare disease in women of reproductive age, although its incidence increases with age [2]. Pyometra is thought to occur as a result of an obstruction to the decreased natural drainage of the uterine cavity. The most common cause of pyometra is gynecologic malignancy. Other benign gynecologic diseases such as leiomyoma, endometrial polyp, congenital anomalies, and atrophic cervicitis can also cause pyometra [3].
The most common symptoms in women presenting with pyometra are abdominal pain, fever and purulent vaginal discharge [2]. A substantial proportion of women with non-ruptured pyometra are asymptomatic [3]. Spontaneous rupture of pyometra is a rare condition that can be misdiagnosed as an acute abdomen associated with perforation of gastrointestinal tract [2, 3]. Colouterine fistula is a rare condition with few cases being reported. The most common cause of colouterine fistula is a complication from colonic diverticulitis [4]. Other causes such as sigmoid malignancy [5], radiotherapy, insertion of intrauterine device [6], endometrial curettage [7], obstetric injury [8, 9] and polymyomectomy [10] have been reported. This is a case report of a colouterine fistula secondary to pyometra.
An 85-year-old woman with severe generalized abdominal pain and malodorous
vaginal discharge for two weeks was admitted to the emergency room of Chonnam
national university hospital. She had no history of endometrial curettage or
insertion of intrauterine device. On physical examination, her abdomen was
slightly distended with the absence of rebound tenderness. She had a blood
pressure of 110/80 mmHg, a pulse rate of 80 beat/min and an axillary temperature
of 36.7
 Fig. 1.
Fig. 1.Abdominopelvic computed tomography showing a suspicious fistula between the sigmoid colon and the uterus (arrow).
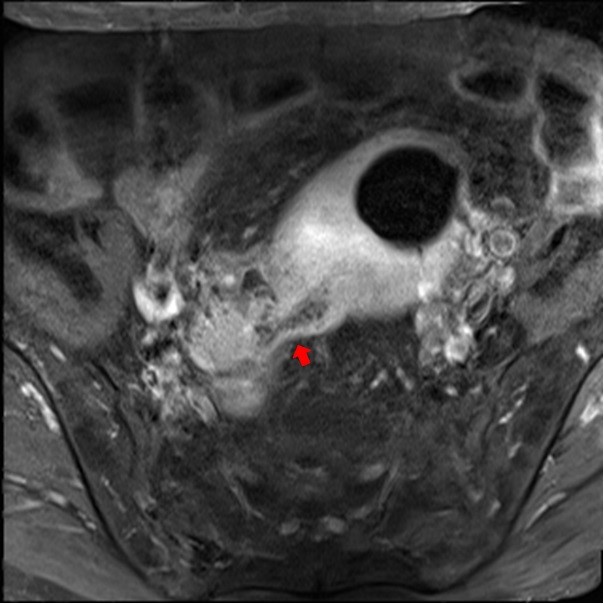 Fig. 2.
Fig. 2.Magnetic resonance imaging showing a fistulous communication between the distal sigmoid colon and the uterine body (arrow) with a widening of the endometrial cavity and presence of air density.
The operation revealed adhesions of the distal sigmoid colon to the uterine posterior wall. Adhesiolysis was performed between the posterior uterine wall and sigmoid colon revealing a 3 mm sized fistula. Total abdominal hysterectomy, bilateral salpingo-oophorectomy, drainage of the abscess and sigmoid colon resection were performed. Histopathological findings of the surgical specimens revealed an atrophic endometrium with acute suppurative inflammation (Fig. 3). The sigmoid colon demonstrated acute serous inflammation showed no evidence for malignancy or diverticulum (Fig. 4). Postoperative recovery was without complications and he was discharged on postoperative day 12.
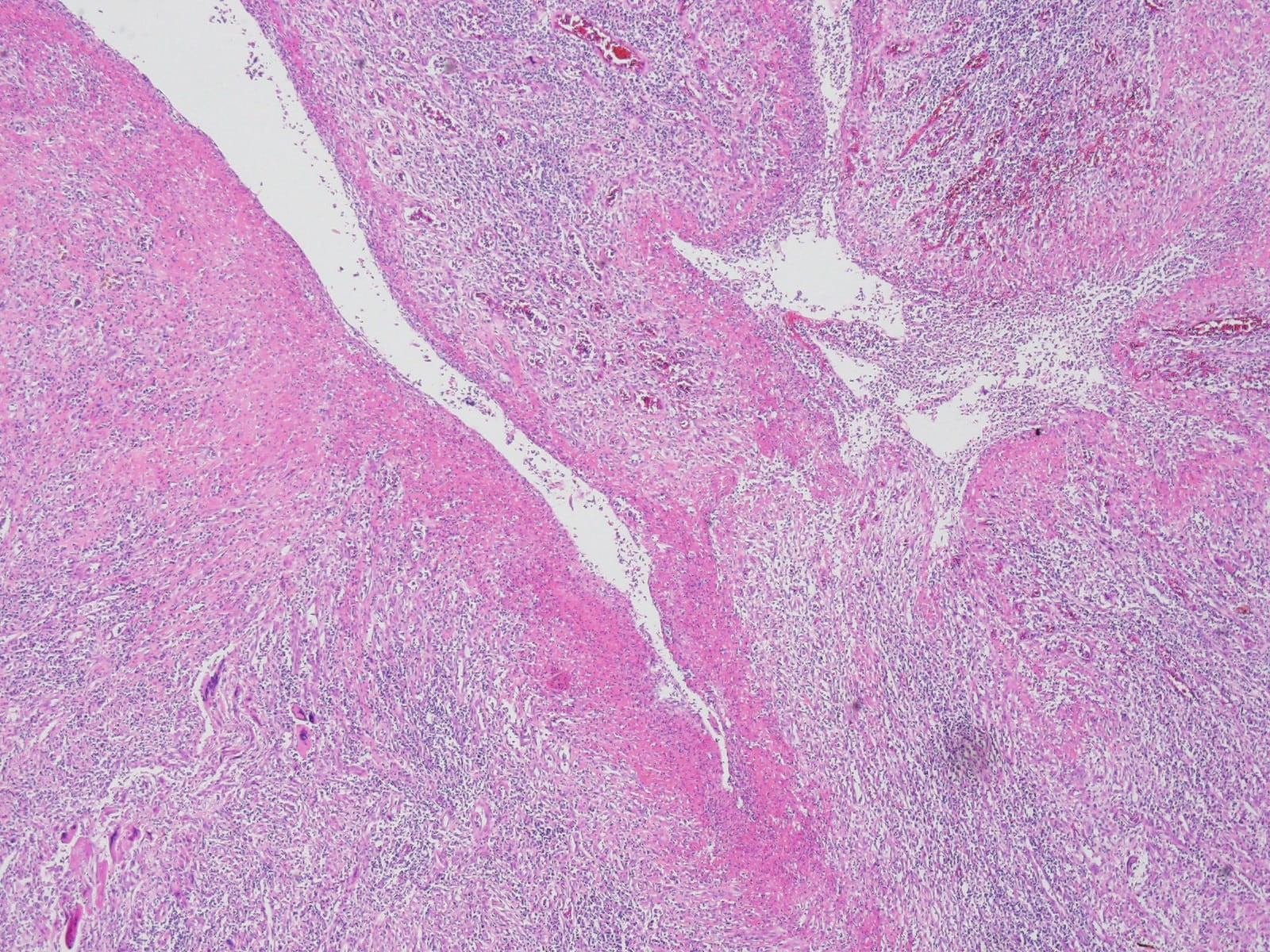 Fig. 3.
Fig. 3.Histopathological sections of Uterus: Endometrial cavity shows
fibrinoid necrosis with acute suppurative inflammation reaction (Hematoxylin &
eosin,
 Fig. 4.
Fig. 4.Histopathological sections of Colon: The slide reveals mild
inflammation in colonic serosa without any tumor cell involvement (Hematoxylin &
eosin
Pyometra, an accumulation of purulent material in the endometrial cavity, is a rare entity in the general population but more common in elderly women [2].
Spontaneous perforation of pyometra is a rare complication with a reported incidence of 0.01–0.5% in gynecologic patients. However, the incidence rises to 13.6% in elderly patients [3]. Unfortunately, it is hard to diagnose Rupture of a pyometra is a difficult diagnosis secondary to the complaints of non-specific symptoms such as fever and abdominal pain. Approximately 16% of patients with ‘perforation of a pyometra are diagnosed preoperatively [11]. Common preoperative diagnoses include generalized peritonitis, pneumoperitoneum and perforation of the gastrointestinal tract [11]. Pyometra can be treated with drainage and antibiotics [12]. However, surgical treatment is often required especially with the presence of perforation of pyometra. Hysterectomy is performed in most women with perforation of a pyometra [2, 3, 11].
We are reporting a case of colouterine fistula secondary to pyometra. Colouterine fistula is an uncommon condition [13]. The majority of cases of colouterine fistula are secondary to the presence of a diverticular abscess extending or rupturing into an adjacent organ [14]. Other causes include sigmoid malignancy [5], radiotherapy, insertion of an intrauterine device [6], endometrial curettage [7], obstetric injury [8, 9] and polymyomectomy [9]. We believe this to be the first reported case of colouterine fistula secondary to pyometra.
Imaging modalities to diagnose colouterine fistula include contrast radiography, ultrasonography, abdominopelvic CT scan and pelvic MRI. Abdominopelvic CT scan is increasingly being used for evaluating acute abdominal pain. Abdominopelvic CT scan is both sensitive and specific in making a diagnosis of diverticulitis [15]. A CT scan is can be helpful in preoperative surgical planning by demonstrating the extent and degree of inflammation. Pelvic MRI is a more accurate diagnostic modality compared to CT scan [16]. MRI has many advantages compared to CT scan, including no ionizing radiation, imaging from almost every angle, with no known associated health risks [16].
Surgical management varies according to the causative pathology. Colouterine fistula caused by malignant disease needs en bloc resection [6]. In the absence of malignancy, the need for hysterectomy has not been established [17]. Because the origin of the causative inflammation is primarily in the colon, resection of the colon with drainage of the uterine cavity might be sufficient [17].
Gynecologists should be aware that pyometra-induced colouterine fistula may occur in elderly patients without colon-origin diseases such as diverticulum or malignancy.
MKC, TYK and CHK designed the study. MKC and TYK collected data and wrote the manuscript. CHK revised the manuscript. All authors read and approved the final manscript.
Written informed consent for the publication of this case was obtained from the patient. The study was conducted in accordance with the Declaration of Helsinki and was approved by the Institutional Review Board at Chonnam National University Hospital (IRB No. CNUH-EXP-2021-083).
We would like to express our gratitude to all those who helped us during the writing of this manuscript.
This research received no external funding.
The authors declare no conflict of interest.
