Introduction: Giant ventral hernia immediately after vaginal twin delivery is a rare event and the management is unclear. Case presentation: A 28-year-old primiparous woman had a spontaneous vaginal preterm twin delivery at gestational age 36 weeks and 5 days, followed by a giant ventral hernia with severe pain. She had a single-incision laparoscopic cholecystectomy two years earlier. She was closely monitored with transfusion and pain control, and improved spontaneously without emergency surgery. Conclusion: Immediately after vaginal twin delivery, a giant ventral hernia was detected in a 28-year-old primiparous woman who had a history of single-incision laparoscopic cholecystectomy. Fortunately, the hernia resolved spontaneously without the need for emergency surgery.
The occurrence of giant ventral hernia after vaginal delivery is an extremely rare event. Due to its rarity, the management options for this condition are not clear. To date, only one case of ventral hernia accompanied by ruptured uterus has been reported and emergency operation was warranted in this situation [1]. Several authors have reported on the association between primary ventral hernia and pregnancy. Pregnancy following hernia repair increases the risk of hernia recurrence by 1.6-fold. Therefore, surgeons generally recommend that the optimal time for elective hernia repair should be deferred until after the last planned pregnancy. Furthermore, parous women carry a seven-fold increased risk of hernia repair compared with nulliparous women [2].
The incidence of incisional hernia after single-incision laparoscopic cholecystectomy is 8%. Compared with conventional laparoscopic cholecystectomy, single-incision laparoscopic cholecystectomy is associated with a higher incidence of incisional hernia [3].
The authors present in this report, a case of a postpartum woman with a giant ventral hernia immediately after vaginal delivery of preterm twins. The patient had a history of single-incision laparoscopic cholecystectomy and her hernia improved without emergency surgery.
The patient was a 28-year-old primiparous woman who had a spontaneous vaginal delivery of preterm twins at 36 weeks and 5 days gestational at a primary hospital. The birthweight of the twins were 2,500 and 2,460 grams, and the APGAR scores were 9/10 and 5/10 (1 min/10 min), respectively. During labor, the woman felt epigastric pain and required pain control, followed by severe pain involving both ribs. The patient experienced no pain relief four hours after delivery despite the administration of ketorolac tromethamine IV. Consequently, the patient was transferred to the author’s hospital.
When the patient arrived at the emergency room, her rib pain numeric rating scale (NRS) score was 7. The patient had a pale appearance. The vital signs were as follows: blood pressure - 90/60 mmHg; respirations - 28 breaths per minute; pulse rate -108 beats per minute; and body temperature -36.8 °C. Physical examination revealed protrusion of abdomen and abdominal tenderness without rebound tenderness. The patient had a history of single-incision laparoscopic cholecystectomy due to chronic cholecystitis at this hospital two years prior. Except for surgical history, there was no other special medical history. The authors performed transabdominal ultrasonography immediately and found minimal fluid collection in both paracolic gutters and no hematoma in the uterus. Initial laboratory findings indicated hemoglobin and hematocrit levels of 9.3 g/dL and 28%, respectively.
One hour after arrival at the emergency room, the patient underwent abdominal and pelvic CT scan, which revealed a copious amount of hemorrhage in the abdomen and multiple intra-abdominal organs (liver, stomach, small and large bowel, and uterus) protruding through the large anterior abdominal wall defect, suggesting hernia (Figure 1). Her severe abdominal pain did not resolve even with opioid analgesics. The authors discussed with the department of general surgery regarding the large ventral hernia and the possibility of strangulation, and suspected that the severe pain might not be related to strangulation, but tears in the abdominal wall muscles. Since her vital signs were soon stabilized with hydration and there was no evidence of strangulation, the authors decided to monitor the patient closely rather than carry out an emergency operation. The patient’s hemoglobin level decreased to 7.5 g/dL by one and a half hours, and was transfused with PRC 1200 cc. The hemoglobin level increased up to 10.4 g/dL, following transfusion.
 Figure 1.
Figure 1.— Liver (left), stomach, small and large bowel (right) protrusion through the abdominal wall defect on the computed tomography.
The authors’ admission plan was close observation including pain control and daily monitoring of hemoglobin levels and abdominal circumference. We decided to administer intravenous tranexamic acid continuously, to control bleeding and also treated the patient with oral methylergometrine maleate as uterotonic three times daily. The authors consulted with the department of anesthesiology and pain medicine about the severe rib pain, and upon their advice, administered continuous patient-controlled anesthesia to relieve the pain. The patient’s hemoglobin levels stabilized immediately upon admission and the abdominal circumference decreased over the next few days to 98, 96, and 93 cm. Furthermore, the patient’s severe abdominal and rib pain was markedly relieved from day 3 of admission, leaving her with only perineal pain, which is a common occurrence in mothers following delivery. Eventually, the patient was discharged after five days of hospitalization.
The patient visited the outpatient department for follow-up a month later and had the appearance of a normal postpartum woman. Transvaginal ultrasonography showed her uterus to measure 82 × 68 × 83 mm with a small myoma and no fluid or hemorrhage in the posterior cul-de-sac. After three months, the patient underwent abdominal and pelvic CT scan, which revealed an improvement in protrusion of intra-abdominal solid organs at the anterior abdominal noted in the previous CT scan (Figure 2). Since her visit to the hospital to review the CT scan results, the patient decided to follow up.
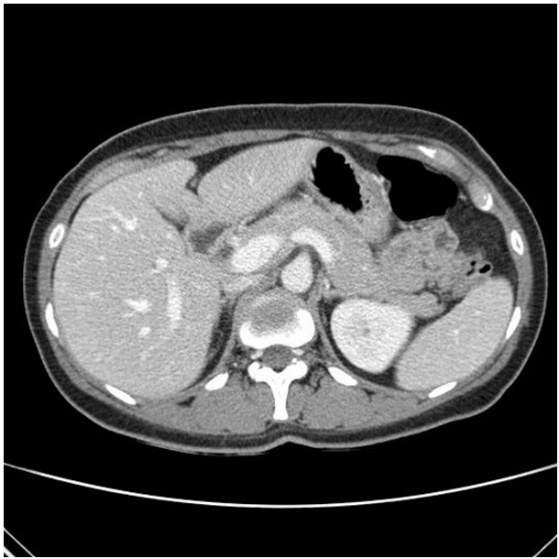 Figure 2.
Figure 2.— Improvement in protrusion of liver, stomach, and large bowel observed on computed tomography scan.
Pregnancy-related ventral hernia is a rare medical condition. Not only is it crucial to effectively time elective hernia repair in women of childbearing age, it is also very important to be accurately estimate the rate of hernia recurrence among this group of women both during and after pregnancy. Because the impact of pregnancy on the risk of recurrence after abdominal hernia repair is unknown, it is advisable to delay repair of ventral hernia until a woman’s last planned pregnancy [4].
The present case involved severe ventral hernia during labor and is considered extremely rare. A similar case was reported by Byun et al. in 2014 [1]. The patient in that case was gravid 2 para 1, delivered full-term vaginally, and had no other specific medical or surgical history. She had a large abdominal wall defect 9 cm in diameter with a ruptured uterus at the right lower portion. She underwent emergency laparotomy including repairs for the ruptured uterine and abdominal wall defects. There are several differences between the case presented by Byun et al. and the patient in the present report. The patient in the present report delivered preterm twins and had no uterine rupture. While the patient presented by Byun et al. had no surgical history, the patient in the present report had previously undergone single-incision laparoscopic surgery. The patient in the present report recovered spontaneously with only close observation and pain management without emergency surgery or any other intervention.
Although not very similar to the present case, a case of perineal hernia after vacuum-assisted vaginal delivery has been reported [5]. The patient had a large bladder hernia through ruptured symphysis pubis and presented with a bulging perineal mass shortly after delivery. She underwent an open reduction and internal fixation for the pubic symphysis diastasis and the symptoms of perineal herniation were not relieved. After a few weeks, she underwent a second surgery known as abdominal-perineal repair. This case differs from the case in the present report in many ways, but shares a common feature involving pelvic organ hernia immediately after vaginal delivery.
The patient in the present report had a history of single-incision laparoscopic cholecystectomy. After single-incision cholecystectomy, the incisional hernia rate was 8% [3]. Also, a higher incidence of incisional hernia was found in patients undergoing single port access cholecystectomy compared with conventional laparoscopic cholecystectomy [6]. Pregnancy, obesity, and chronic cough strain the abdominal wall and are therefore risk factors for hernia [7]. In the patient presented in the current report, a history of single-incision cholecystectomy and twin pregnancy likely increased the risk of giant ventral hernia.
In twins between gestational ages 32-38 weeks, planned cesaran section offers no significant benefits over vaginal delivery in a situation where the first twin is in the cephalic position. In terms of maternal morbidity and mortality, there were no significant differences between planned cesarean section and vaginal delivery in twin pregnancy [8]. A cesarean delivery might have been more advantageous than vaginal delivery in the present patient.
Giant ventral hernia after vaginal delivery as presented in this case is quite rare. The patient resolved spontaneously with close clinical monitoring. The severe rib pain was controlled with continuous patient-controlled anesthesia. This case report contributes to our knowledge on the management of giant ventral hernia after vaginal delivery.
All subjects gave their informed consent for inclusion before they participated in the study. The study was conducted in accordance with the Declaration of Helsinki.
Thanks to all the peer reviewers and editors for their opinions and suggestions.
The authors declare no conflict of interest.
